Adenoids

Adenoids
Adenoids are part of the lymphatic system and are located at the back of the nasal cavity, above the tonsils. These small structures play a role in immune function, particularly during childhood, helping to trap bacteria and viruses that enter the body through the nose. Understanding the symptoms, causes, and types of adenoid-related issues is crucial for proper diagnosis and management.
Symptoms:
- Nasal Congestion: Adenoid enlargement can lead to nasal congestion, making breathing through the nose difficult.
- Breathing Through the Mouth: Due to nasal congestion, individuals, especially children, may breathe primarily through their mouths.
- Snoring: Enlarged adenoids can contribute to snoring during sleep.
- Sleep Apnea: Severe adenoid enlargement may lead to sleep apnea, characterized by pauses in breathing during sleep.
- Ear Infections: Adenoids can block the Eustachian tubes, leading to fluid accumulation in the middle ear and increasing the risk of ear infections.
- Runny Nose: Chronic nasal discharge may be present.
- Swallowing Issues: In some cases, enlarged adenoids can affect swallowing and lead to a sensation of a lump in the throat.
Causes:
The primary cause of adenoid issues is enlargement, often due to infections. Factors contributing to adenoid enlargement include:
- Infections: Recurrent infections, particularly in childhood, can lead to adenoid hypertrophy.
- Allergies: Persistent exposure to allergens may contribute to adenoid enlargement.
- Genetics: Some individuals may be predisposed to adenoid issues due to genetic factors.
- Immune System Response: Adenoids can enlarge as part of the body’s immune response to infections.
Types of Adenoid Issues:
- Adenoid Hypertrophy: Enlargement of the adenoids due to recurrent infections or other factors, leading to symptoms such as nasal congestion and breathing difficulties.
- Adenoiditis: Inflammation of the adenoids, often caused by bacterial or viral infections, resulting in symptoms like a runny nose, sore throat, and difficulty swallowing.
- Obstructive Sleep Apnea: Severe adenoid enlargement can obstruct the airway during sleep, causing pauses in breathing and disrupting sleep patterns.
- Chronic Otitis Media: Enlarged adenoids can block the Eustachian tubes, contributing to fluid accumulation in the middle ear and increasing the risk of chronic ear infections.
- Adenoid Cystic Carcinoma: A rare and malignant tumor that can develop in the adenoids. This type of cancer requires specialized medical attention.
Adenoids are important immune structures located in the back of the nasal cavity. Enlargement of the adenoids can lead to various symptoms, and understanding the causes and types of adenoid-related issues is crucial for effective management. Seeking medical advice is essential for proper diagnosis and the development of a personalized treatment plan.
Deviated Septum
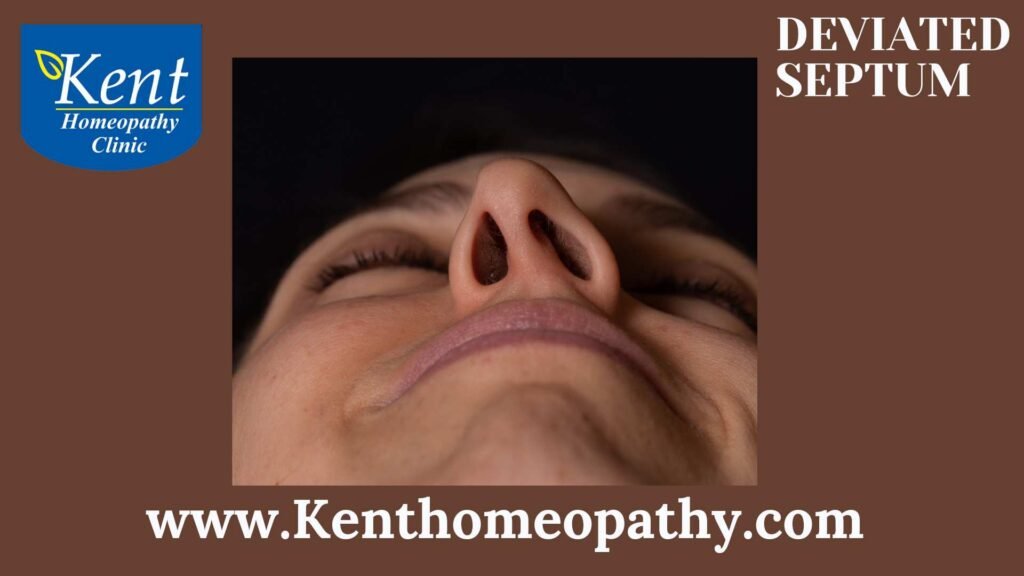
Deviated Septum
A deviated septum is a common anatomical condition in which the thin wall (nasal septum) that separates the nostrils is displaced or deviates to one side. This deviation can vary in severity and may lead to a variety of symptoms affecting breathing and overall nasal function. Understanding the symptoms, causes, and types of a deviated septum is crucial for those experiencing nasal issues.
Symptoms:
The symptoms of a deviated septum can vary among individuals, and not everyone with a deviated septum will experience noticeable effects. Common symptoms include:
- Nasal Congestion: Deviated septum can restrict airflow through one or both nostrils, leading to chronic nasal congestion. Individuals may feel like one side of the nose is more congested than the other.
- Nosebleeds: The altered airflow and drying of nasal passages can make individuals more prone to nosebleeds. The deviated septum may expose blood vessels to drying air, increasing the risk of bleeding.
- Facial Pain or Headaches: Displacement of the septum can cause pressure imbalances in the nasal area, leading to facial pain or headaches, especially if there is obstruction of sinus drainage.
- Snoring: The altered airflow due to a deviated septum can contribute to snoring, particularly during sleep. It may result from increased turbulence in the airflow.
- Frequent Sinus Infections: Difficulty in draining mucus from the affected side can lead to the accumulation of mucus, providing a conducive environment for bacterial growth and increasing the risk of sinus infections.
- Postnasal Drip: Excess mucus production on one side may result in postnasal drip, where mucus drips down the back of the throat, causing irritation and cough.
- Sleep Disturbances: Breathing difficulties during sleep, especially when lying on one side, may lead to disrupted sleep patterns, contributing to fatigue.
Causes:
Several factors contribute to the development of a deviated septum, and the condition can result from a combination of these factors:
- Congenital Deviation: Some individuals are born with a deviated septum due to irregularities in the fetal development process. It may become more apparent as a person grows.
- Trauma or Injury: Physical trauma to the nose, such as a broken nose from accidents, falls, or sports injuries, can cause the septum to deviate. Trauma may displace the cartilage or bone that makes up the septum.
- Aging: The septum can naturally change shape over time due to the aging process, leading to a deviated septum, particularly in older individuals.
Types:
Deviated septum types refer to the variations in the deviation pattern, and they can impact the severity of symptoms. Common types include:
- C-Shaped Deviation: The septum is bent in the shape of a “C,” causing obstruction on one side. This type of deviation often results in more noticeable symptoms due to the pronounced curvature.
- S-Shaped Deviation: The septum takes on an “S” shape, which can lead to more complex nasal obstruction. Individuals with an S-shaped deviation may experience varying degrees of nasal congestion on both sides.
- Spur Formation: In addition to lateral deviation, bony spurs or projections may develop on the septum, contributing to the overall deviation and affecting airflow. Spurs can exacerbate symptoms such as nasal congestion and postnasal drip.
- Posterior Deviation: In some cases, the back part of the septum, near the throat, is displaced, affecting the passage of air through the nasal cavity. This type of deviation can contribute to sleep disturbances and snoring.
ENT Treatment

ENT Treatment
Ear, Nose, and Throat (ENT) treatment, also known as otolaryngology, focuses on the medical and surgical management of disorders and conditions affecting the ears, nose, throat, and related structures in the head and neck. ENT specialists, or otolaryngologists, address a wide range of issues, from common infections to complex surgical procedures.
Symptoms:
- Hearing Loss: Both sudden and gradual hearing loss can be indicative of various ear-related issues.
- Ear Pain: Pain or discomfort in the ear may be caused by infections, injury, or other underlying conditions.
- Sinus Congestion: Chronic sinus congestion or nasal obstruction can lead to breathing difficulties and recurrent sinus infections.
- Throat Pain: Persistent throat pain, difficulty swallowing, or the sensation of a lump in the throat may be signs of throat-related disorders.
- Snoring and Sleep Apnea: These issues often involve the structures of the nose and throat, impacting breathing during sleep.
- Vertigo: Dizziness or a spinning sensation can be related to inner ear problems affecting balance.
- Chronic Cough: A persistent cough may be associated with conditions affecting the throat or respiratory system.
Causes:
- Infections: Bacterial or viral infections can affect the ears, nose, and throat, leading to symptoms like pain, congestion, and discharge.
- Allergies: Allergic reactions can cause sinus congestion, sneezing, and other symptoms affecting the ears, nose, and throat.
- Structural Abnormalities: Anatomical issues such as deviated septum, nasal polyps, or enlarged tonsils can contribute to ENT problems.
- Gastroesophageal Reflux Disease (GERD): Stomach acid refluxing into the throat can cause irritation, leading to symptoms like chronic cough or throat discomfort.
- Environmental Factors: Exposure to pollutants, irritants, or secondhand smoke can contribute to ENT issues.
Types:
- Otology/Neurotology: Focuses on the ear and related neurological structures, addressing conditions like hearing loss, ear infections, and disorders affecting balance.
- Rhinology: Specializes in disorders of the nose and sinuses, including sinusitis, nasal polyps, and nasal obstruction.
- Laryngology: Deals with disorders of the larynx (voice box) and throat, addressing conditions like vocal cord nodules, hoarseness, and swallowing disorders.
- Head and Neck Surgery: Involves the surgical treatment of tumors, infections, or deformities in the head and neck region.
- Pediatric Otolaryngology: Concentrates on ENT issues affecting children, including ear infections, tonsillitis, and congenital abnormalities.
- Facial Plastic and Reconstructive Surgery: Focuses on cosmetic and reconstructive procedures related to the head and neck.
ENT treatment aims to address a wide range of disorders affecting the ears, nose, throat, and related structures. Early diagnosis and appropriate management by ENT specialists are crucial for optimal outcomes and improved quality of life.
Hoarseness
Hoarseness
Hoarseness: Understanding Symptoms, Causes, and Types
Hoarseness is a common symptom characterized by an abnormal change in the voice quality, making it sound rough, raspy, or strained. It is often associated with changes in the vocal cords or the surrounding structures that affect their normal function. Understanding the symptoms, causes, and types of hoarseness is essential for accurate diagnosis and appropriate management.
Symptoms:
- Altered Voice Quality: The primary symptom is a noticeable change in the voice, which may sound rough, breathy, or strained.
- Pitch Changes: Hoarseness can lead to variations in pitch, making the voice sound higher or lower than usual.
- Voice Fatigue: Prolonged speaking or singing may result in quicker voice fatigue.
- Throat Pain or Discomfort: Some individuals with hoarseness may experience pain, discomfort, or a sensation of a lump in the throat.
- Coughing or Clearing the Throat: Persistent throat clearing or coughing can be associated with hoarseness.
- Difficulty Swallowing: In some cases, hoarseness may be accompanied by difficulty swallowing or a feeling of tightness in the throat.
Causes:
Several factors can contribute to the development of hoarseness, including:
- Vocal Cord Nodules or Polyps: Noncancerous growths on the vocal cords, often caused by vocal abuse or misuse.
- Acid Reflux (Gastroesophageal Reflux Disease – GERD): Stomach acid backing up into the throat can irritate and damage the vocal cords.
- Viral Infections: Respiratory infections, such as colds or flu, can lead to inflammation of the vocal cords.
- Bacterial Infections: Infections affecting the larynx or surrounding structures may cause hoarseness.
- Voice Overuse or Misuse: Excessive talking, yelling, or singing without proper vocal technique can strain the vocal cords.
- Smoking: Tobacco smoke irritates the vocal cords and can contribute to chronic hoarseness.
- Neurological Conditions: Disorders affecting the nerves controlling the vocal cords, such as Parkinson’s disease or certain strokes.
- Thyroid Disorders: An underactive or overactive thyroid can impact voice quality.
- Trauma or Injury: Injuries to the larynx or vocal cords, often resulting from accidents or surgery.
- Allergies: Persistent postnasal drip due to allergies can irritate the vocal cords.
- Laryngopharyngeal Reflux (LPR): Similar to GERD, LPR involves stomach acid affecting the throat and vocal cords.
- Tumors: Benign or malignant growths on the vocal cords or in the throat can lead to hoarseness.
Types:
- Functional Hoarseness: Often related to vocal abuse, misuse, or overuse without structural changes to the vocal cords.
- Organic Hoarseness: Caused by structural abnormalities or diseases affecting the vocal cords or surrounding structures. Examples include nodules, polyps, or tumors.
- Psychogenic Hoarseness: Hoarseness without evident physical or structural causes, often related to psychological factors.
Mastoiditis
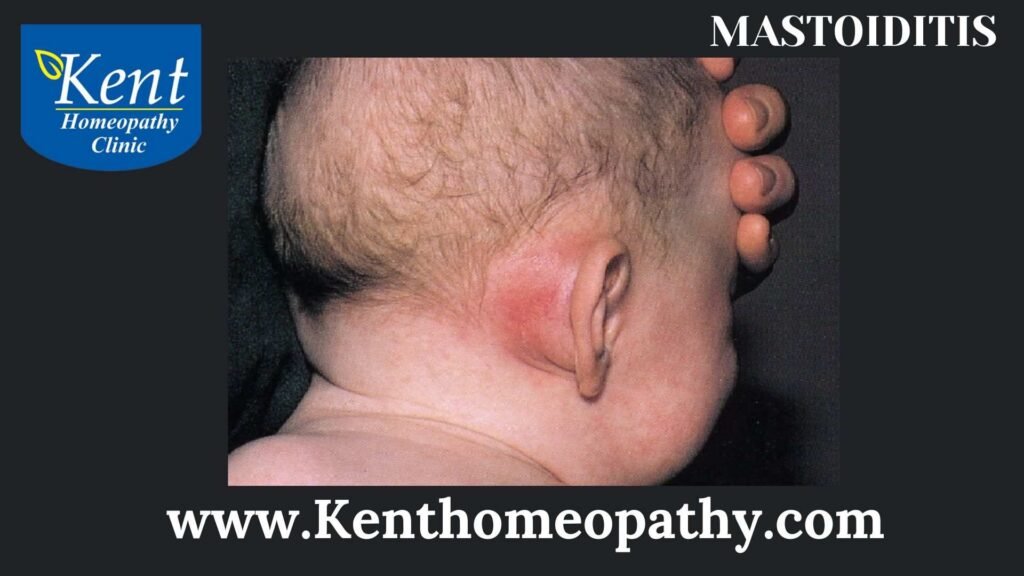
Mastoiditis
Mastoiditis: Understanding Symptoms, Causes, and Types
Mastoiditis is a bacterial infection of the mastoid bone, a prominent bone behind the ear. It often develops as a complication of untreated or inadequately treated middle ear infections (otitis media). Mastoiditis can lead to inflammation, pain, and potential complications, making prompt diagnosis and appropriate treatment essential.
Symptoms:
- Ear Pain:
– Persistent or severe ear pain is a common symptom, often localized to the affected ear.
- Ear Discharge:
– Pus or other discharge from the ear may be present, indicating an infection in the middle ear.
- Hearing Loss:
– Hearing loss can occur due to the inflammation and infection affecting the structures of the ear.
- Swelling Behind the Ear:
– Swelling and redness may be visible behind the affected ear, where the mastoid bone is located.
- Fever:
– Elevated body temperature, fever, is a typical response to infection.
- Headache:
– Headaches, particularly localized around the affected ear, may occur.
- Fatigue:
– Generalized weakness and fatigue are common symptoms, reflecting the body’s response to infection.
- Irritability (in children):
– Children with mastoiditis may exhibit irritability, fussiness, or difficulty sleeping.
Causes:
- Middle Ear Infections (Otitis Media):
– Mastoiditis often arises as a complication of untreated or inadequately treated middle ear infections. Bacteria from the middle ear can spread to the mastoid bone.
- Blockage of the Eustachian Tube:
– The Eustachian tube connects the middle ear to the back of the nose. Blockage of this tube can trap bacteria in the middle ear, leading to infection and potential spread to the mastoid.
- Respiratory Infections:
– Infections such as respiratory tract infections or colds can contribute to the development of middle ear infections and, subsequently, mastoiditis.
- Immunocompromised State:
– Individuals with compromised immune systems, due to conditions like HIV/AIDS or certain medical treatments, may be more susceptible to mastoiditis.
Types of Mastoiditis:
- Acute Mastoiditis:
– This is the initial stage of infection, characterized by rapid onset of symptoms. Prompt treatment is crucial to prevent complications.
- Subacute Mastoiditis:
– If acute mastoiditis is not promptly treated, the infection may progress to a subacute stage with persistent symptoms and a greater risk of complications.
- Chronic Mastoiditis:
– Long-term or recurrent infections may lead to chronic mastoiditis, marked by ongoing inflammation and potential damage to the mastoid bone and surrounding structures.
- Complicated Mastoiditis:
– Complications can arise if the infection spreads to nearby structures, such as the inner ear, facial nerve, or brain. This can result in more severe symptoms and potential life-threatening complications.
It’s crucial to seek medical attention promptly if symptoms of mastoiditis, such as ear pain, discharge, or swelling, are present. Early diagnosis and appropriate treatment help prevent the progression of the infection and reduce the risk of complications. Parents should be particularly vigilant about recognizing signs of ear infections in children to initiate timely intervention.
In conclusion, mastoiditis is a potentially serious condition that can result from untreated middle ear infections. Understanding its symptoms, causes, and types is essential for early detection and appropriate management. With prompt medical intervention, including antibiotic therapy and, if necessary, surgical procedures, the majority of individuals with mastoiditis can achieve a full recovery.
Nasal Polyps

Nasal Polyps
Nasal Polyps: Unveiling Symptoms, Causes, and Types
Nasal polyps are soft, non-cancerous growths that develop on the lining of the nasal passages or sinuses. These polyps are often associated with chronic inflammation and can vary in size, causing symptoms such as nasal congestion, loss of smell, and facial pressure. Understanding the symptoms, causes, and types of nasal polyps is crucial for effective management and treatment.
Symptoms:
- Nasal Congestion: One of the primary symptoms of nasal polyps is nasal congestion or blockage. The polyps can obstruct normal airflow through the nasal passages, leading to difficulty breathing through the nose.
- Runny Nose: Persistent runny nose or rhinorrhea is common. The nasal discharge is often thin and clear but may become thicker if a secondary infection develops.
- Postnasal Drip: Excess mucus produced by the polyps can result in postnasal drip, where mucus drips down the back of the throat, leading to throat irritation and cough.
- Loss of Smell: Nasal polyps can interfere with the sense of smell (anosmia) or taste due to the blockage of odor-carrying particles.
- Facial Pressure: Some individuals with nasal polyps may experience facial pressure or pain, particularly around the eyes or in the cheeks. This can be more pronounced during sinus infections.
- Snoring: Enlarged nasal polyps may contribute to snoring by narrowing the air passages during sleep.
- Headache: Persistent or recurrent headaches may occur in individuals with nasal polyps, especially if sinus infections are present.
- Itchy Eyes: Irritation of the eyes, including itching and watering, can result from the drainage of mucus into the throat and eyes.
- Coughing: Chronic coughing may be a symptom, often related to postnasal drip or irritation of the airways.
Causes:
- Chronic Inflammation: Nasal polyps are closely associated with chronic inflammation of the nasal mucosa and sinuses. This inflammation can be triggered by various factors, including allergies, infections, or environmental irritants.
- Allergic Rhinitis: Individuals with allergic rhinitis, commonly known as hay fever, are more prone to developing nasal polyps. Allergies can contribute to persistent inflammation in the nasal passages.
- Asthma: There is a recognized association between nasal polyps and asthma. Individuals with asthma are at an increased risk of developing nasal polyps, and vice versa.
- Aspirin Sensitivity (Aspirin-Exacerbated Respiratory Disease – AERD): Some people with nasal polyps may have an increased sensitivity to aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs).
- Genetic Factors: There may be a genetic predisposition to developing nasal polyps, as they can run in families.
- Cystic Fibrosis: Nasal polyps are more prevalent in individuals with cystic fibrosis, a genetic disorder affecting the respiratory and digestive systems.
- Age: While nasal polyps can occur at any age, they are more common in adults, especially those over the age of 40.
- Immune System Disorders: Conditions that affect the immune system, such as primary immunodeficiency disorders, may increase the risk of nasal polyps.
Types:
- Ethmoidal Polyps:
– Location: Found in the ethmoid sinuses, which are air-filled spaces between the eyes.
– Characteristics: These polyps often arise from the ethmoid sinuses and can extend into the nasal passages.
- Antrochoanal Polyps:
– Location: Originating from the maxillary sinuses.
– Characteristics: Antrochoanal polyps grow into the nasal passages and may extend into the throat.
- Multiple Polyps (Polyposis):
– Characteristics: Individuals with nasal polyposis develop multiple polyps in the nasal and sinus cavities.
– Association: Often associated with conditions like asthma, aspirin sensitivity, and chronic sinusitis.
- Inverted Papilloma:
– Characteristics: While not a true polyp, inverted papillomas are benign growths that can affect the nasal lining.
– Risk: Although rare, inverted papillomas have the potential for more aggressive behavior than typical nasal polyps.
- Allergic Fungal Sinusitis (AFS):
– Characteristics: Associated with the presence of fungi in the sinuses, often seen in individuals with allergies.
– Symptoms: Chronic sinusitis symptoms, nasal polyps, and an eosinophilic inflammatory response.
Tinnitus
Tinnitus
Tinnitus: Unraveling Symptoms, Causes, and Types
Tinnitus is a condition characterized by the perception of noise in the ears or head when no external sound source is present. This auditory phenomenon can vary in intensity and duration, affecting millions of people globally. Understanding the symptoms, causes, and types of tinnitus is essential for managing this often persistent and bothersome condition.
Symptoms:
- Ringing, Buzzing, or Hissing Sounds:
– The hallmark symptom of tinnitus is the perception of sounds that aren’t external to the body. These sounds can manifest as ringing, buzzing, hissing, whistling, or even roaring noises.
- Constant or Intermittent:
– Tinnitus may be constant, where the sound is present without cessation, or intermittent, with periods of silence between episodes.
- Unilateral or Bilateral:
– Tinnitus can affect one ear (unilateral) or both ears (bilateral). The nature and characteristics of the perceived sounds may differ between ears.
- Associated Hearing Loss:
– Some individuals with tinnitus may experience concurrent hearing loss. The severity of hearing loss can vary, and it may be more pronounced at certain frequencies.
- Impact on Concentration and Sleep:
– Tinnitus can interfere with concentration and sleep, affecting an individual’s overall quality of life. The constant presence of internal sounds can be distressing for some.
- Pulsatile Tinnitus:
– In some cases, individuals may experience pulsatile tinnitus, where the perceived sound synchronizes with the heartbeat. This can be associated with vascular issues.
Causes:
- Noise-Induced Hearing Loss:
– Exposure to loud noises, whether from occupational settings, recreational activities, or traumatic events, can damage the delicate structures of the inner ear and lead to tinnitus.
- Age-Related Hearing Loss:
– Age-related hearing loss, known as presbycusis, can contribute to tinnitus. As individuals age, the auditory system undergoes changes that may lead to both hearing loss and tinnitus.
- Earwax Blockage:
– Accumulation of earwax in the ear canal can obstruct sound transmission and cause tinnitus. Removal of excess earwax may alleviate symptoms.
- Meniere’s Disease:
– Meniere’s disease is a disorder of the inner ear that can cause vertigo, hearing loss, and tinnitus. It is associated with fluid imbalance in the inner ear.
- Ototoxic Medications:
– Certain medications, termed ototoxic, have the potential to damage the auditory system and cause tinnitus. These may include some antibiotics, diuretics, and cancer medications.
- Temporomandibular Joint (TMJ) Disorders:
– Dysfunction of the temporomandibular joint, which connects the jaw to the skull, can lead to tinnitus. The close proximity of the jaw joint to the ear may contribute to auditory symptoms.
- Head and Neck Injuries:
– Trauma to the head or neck, such as a concussion or whiplash, can affect the auditory system and result in tinnitus.
- Vascular Disorders:
– Certain vascular conditions, including high blood pressure and turbulent blood flow, can cause pulsatile tinnitus, where the perceived sounds synchronize with the heartbeat.
- Infections and Diseases:
– Infections of the ear or diseases affecting the auditory system, such as acoustic neuroma, may contribute to tinnitus.
- Stress and Anxiety:
– Emotional factors like stress and anxiety can exacerbate tinnitus or contribute to its onset. The interaction between psychological factors and tinnitus is complex.
Types:
- Subjective Tinnitus:
– Subjective tinnitus is the most common type, where only the person experiencing it can hear the internal sounds. It is often associated with noise-induced hearing loss, age-related hearing loss, or various underlying conditions.
- Objective Tinnitus:
– Objective tinnitus is less common and occurs when both the person with tinnitus and others can hear the internal sounds. This type is often associated with vascular issues, muscle spasms in the middle ear, or abnormalities in the auditory system.
- Pulsatile Tinnitus:
– Pulsatile tinnitus is characterized by rhythmic sounds that coincide with the heartbeat. It is often associated with vascular conditions, such as high blood pressure, turbulent blood flow, or vascular tumors.
- Somatic Tinnitus:
– Somatic tinnitus is influenced by movements or palpations of the head, neck, or jaw. Changes in posture or muscle contractions may modulate the intensity or characteristics of the perceived sounds.
- Neurological Tinnitus:
– Neurological tinnitus is associated with disorders affecting the nervous system, such as multiple sclerosis or traumatic brain injuries. It involves alterations in the neural pathways involved in auditory perception.
Tonsillitis

Tonsillitis
Tonsillitis: Unraveling Symptoms, Causes, and Types
Tonsillitis is the inflammation of the tonsils, which are two oval-shaped pads of tissue located at the back of the throat. This condition is commonly seen in children but can affect individuals of any age. Understanding the symptoms, causes, and types of tonsillitis is essential for proper diagnosis and effective management.
Symptoms:
- Sore Throat:
– A sore throat is a hallmark symptom of tonsillitis. The throat may be red and swollen, causing discomfort and pain, especially while swallowing.
- Difficulty Swallowing:
– Due to the inflammation of the tonsils and surrounding tissues, individuals with tonsillitis may experience difficulty or pain while swallowing.
- Swollen Tonsils:
– Swelling of the tonsils is a noticeable symptom. In severe cases, the tonsils may become so enlarged that they obstruct the throat, leading to breathing difficulties.
- Red Tonsils with White or Yellow Patches:
– The tonsils may appear red, and there may be white or yellow patches or coatings on their surface, indicating the presence of pus.
- Bad Breath:
– Bad breath (halitosis) is a common symptom due to the accumulation of bacteria and debris in the inflamed tonsils.
- Fever:
– Tonsillitis can be accompanied by a fever. The body’s immune response to the infection can elevate the body temperature.
- Headache and Earache:
– Headaches and earaches may occur as secondary symptoms of tonsillitis, adding to the overall discomfort.
- Fatigue:
– The body’s efforts to fight the infection can lead to fatigue and general feelings of weakness.
Causes:
- Viral Infections:
– The majority of tonsillitis cases are caused by viral infections, with common culprits being the rhinovirus, adenovirus, influenza virus, and the Epstein-Barr virus.
- Bacterial Infections:
– Bacterial infections, particularly by Streptococcus pyogenes (group A streptococcus), are another common cause of tonsillitis. This type of bacterial infection is known as strep throat.
- Common Cold and Respiratory Infections:
– Tonsillitis can develop as a complication of common colds or other respiratory infections when viruses or bacteria spread to the tonsils.
- Infectious Mononucleosis (Mono):
– The Epstein-Barr virus, which causes infectious mononucleosis (mono), is a viral infection that can lead to severe tonsillitis.
- Environmental Factors:
– Exposure to environmental irritants, such as tobacco smoke or pollution, can contribute to the inflammation of the tonsils.
Types:
- Acute Tonsillitis:
– Acute tonsillitis is the most common form and is characterized by a sudden onset of symptoms. It can be caused by either viral or bacterial infections.
- Chronic Tonsillitis:
– Chronic tonsillitis involves persistent inflammation of the tonsils and is often associated with recurrent or prolonged episodes of acute tonsillitis. It can affect daily life and may require more extensive management.
- Recurrent Tonsillitis:
– Recurrent tonsillitis refers to multiple episodes of acute tonsillitis within a year. This condition may be associated with chronic inflammation and can lead to considerations for tonsillectomy (surgical removal of the tonsils).
- Strep Throat:
– Strep throat is a specific type of tonsillitis caused by infection with Streptococcus pyogenes bacteria. It is important to diagnose and treat strep throat promptly to prevent potential complications.
- Peritonsillar Abscess:
– In some cases, tonsillitis can lead to the formation of a peritonsillar abscess, which is a collection of pus near the tonsils. This can cause severe pain, difficulty opening the mouth, and may require drainage.
Vocal Nodules

Vocal Nodules
Vocal Nodules: Unravelling Symptoms, Causes, and Types
Vocal nodules, also known as vocal cord nodules or singer’s nodes, are noncancerous growths that form on the vocal cords. They often develop as a result of vocal strain or misuse and can affect individuals of all ages, though they are more commonly seen in those who use their voices extensively. Understanding the symptoms, causes, and types of vocal nodules is crucial for proper diagnosis and management.
Symptoms:
- Hoarseness:
– Persistent hoarseness is a hallmark symptom of vocal nodules. The voice may sound breathy, rough, or strained.
- Pitch Changes:
– Individuals with vocal nodules may experience changes in pitch, making it difficult to maintain a consistent voice.
- Voice Fatigue:
– Vocal fatigue, characterized by a tired or strained feeling in the throat after speaking or singing for a short period, is common with vocal nodules.
- Pain or Discomfort:
– Pain or discomfort in the throat may be present, especially during or after speaking or singing.
- Reduced Vocal Range:
– Vocal nodules can lead to a reduced vocal range, making it challenging to hit certain pitches or produce specific sounds.
- Throat Clearing:
– Frequent throat clearing is a compensatory behavior that individuals with vocal nodules may adopt in an attempt to alleviate irritation.
- Difficulty Projecting Voice:
– Individuals may find it difficult to project their voice, leading to a weaker and less audible sound.
Causes:
- Vocal Strain and Overuse:
– The primary cause of vocal nodules is vocal strain and overuse. This often occurs in individuals who use their voices extensively, such as singers, teachers, or call center professionals.
- Incorrect Vocal Techniques:
– Poor vocal techniques, including incorrect breathing, improper pitch, and straining the vocal cords, can contribute to the development of nodules.
- Repetitive Trauma:
– Continuous and repetitive trauma to the vocal cords, often from habits like shouting or speaking loudly for extended periods, can lead to the formation of nodules.
- Gastroesophageal Reflux Disease (GERD):
– GERD, a condition where stomach acid flows back into the esophagus, can irritate the vocal cords and contribute to the development of nodules.
- Smoking:
– Smoking and exposure to secondhand smoke can irritate and inflame the vocal cords, increasing the risk of developing nodules.
- Dehydration:
– Inadequate hydration can lead to dryness and irritation of the vocal cords, making them more susceptible to injury and nodule formation.
- Vocal Fold Haemorrhage:
– In some cases, a vocal fold haemorrhage, which is bleeding into the vocal cord, can contribute to the development of nodules.
Types:
- Acute Vocal Nodules:
– Acute vocal nodules develop suddenly due to a specific episode of vocal strain or trauma. This type is often associated with a recent increase in vocal demands.
- Chronic Vocal Nodules:
– Chronic vocal nodules develop gradually over time due to ongoing vocal misuse or overuse. This type is more common in individuals with long-term vocal habits that strain the vocal cords.
- Singer’s Nodules:
– Singer’s nodules specifically affect individuals who use their voices professionally, such as singers and performers. These nodules often develop due to the demands of their vocal profession.
- Teacher’s Nodules:
– Teacher’s nodules are common in educators who engage in prolonged speaking in noisy environments, leading to chronic vocal strain and the development of nodules.
- Childhood Vocal Nodules:
– Vocal nodules can also affect children, often due to excessive shouting, screaming, or talking loudly. This type requires special consideration in diagnosis and management.
Contact to know more
Contact
Timings
Monday to Saturday:
11:00 AM to 02:30 PM
06:30 PM to 09:00 PM
