Fever

Fever
Fever is a common physiological response to infection, inflammation, or certain medical conditions. It involves an elevation of body temperature above the normal range, typically around 98.6°F (37°C). Fever is a complex process regulated by the body’s thermostat, the hypothalamus, and is often a sign that the immune system is actively responding to an underlying threat.
Symptoms:
- Elevated Body Temperature: The hallmark symptom of fever is an increase in body temperature. A fever is generally defined as a body temperature higher than 100.4°F (38°C).
- Chills and Shivering: Many individuals with fever experience chills and shivering as the body tries to generate and conserve heat.
- Headache: Fever can be accompanied by a headache, contributing to overall discomfort.
- Muscle Aches: Generalized muscle aches and weakness are common during a fever.
- Sweating: As the body temperature rises, sweating may occur as a cooling mechanism.
Causes:
- Infections: Most fevers are a response to infections caused by bacteria, viruses, fungi, or parasites.
- Inflammatory Conditions: Non-infectious inflammatory conditions, such as rheumatoid arthritis or inflammatory bowel diseases, can lead to fever.
- Heat-related Illnesses: Exposure to extreme heat, leading to conditions like heatstroke, can cause fever.
- Certain Medications: Some medications may induce fever as a side effect.
- Autoimmune Disorders: Conditions where the immune system mistakenly attacks the body’s own tissues can result in fever.
- Cancer: Certain cancers, particularly blood cancers like leukemia, can cause fever.
Types:
- Low-Grade Fever: Body temperature slightly above the normal range, usually up to 100.4°F (38°C).
- Moderate Fever: Body temperature ranging from 100.4°F (38°C) to 102.2°F (39°C).
- High Fever: Body temperature exceeding 102.2°F (39°C).
- Intermittent Fever: Fever that comes and goes at regular intervals.
- Remittent Fever: Continuous fever with fluctuations exceeding 2°F (1.1°C) but remaining above normal.
- Pel-Ebstein Fever: A specific type of fever pattern seen in some cases of Hodgkin’s lymphoma, characterized by fever spikes lasting several days followed by afebrile periods.
While fever itself is generally not harmful and often indicates the body’s defense mechanisms in action, persistent or high fevers may warrant medical attention. Seeking medical advice is crucial, especially if fever is accompanied by severe symptoms, lasts for an extended period, or occurs in vulnerable populations such as young children or the elderly.
General Medical Consultation

General Medical Consultation
A general medical consultation refers to a comprehensive evaluation and discussion between a patient and a medical professional, typically a primary care physician or general practitioner. During this consultation, the physician assesses the patient’s health, discusses symptoms, and may order diagnostic tests to arrive at a diagnosis or provide guidance on further medical care.
Symptoms:
General medical consultations can cover a wide range of symptoms, as patients seek guidance for various health concerns. Common symptoms that may prompt individuals to seek a general medical consultation include:
- Fever: Persistent or recurring fevers may indicate infections or underlying health issues that require evaluation.
- Pain: Any unexplained or chronic pain, whether localized or widespread, is a common reason for seeking medical advice.
- Fatigue: Persistent fatigue or exhaustion that interferes with daily activities may be a sign of various medical conditions.
- Respiratory Issues: Symptoms such as cough, shortness of breath, or chest pain may prompt individuals to seek consultation for respiratory conditions.
- Digestive Problems: Issues like persistent nausea, vomiting, diarrhea, abdominal pain, or changes in bowel habits may lead to medical consultations.
- Skin Conditions: Rashes, lesions, or any concerning changes in skin appearance may necessitate a consultation.
- Mental Health Concerns: Anxiety, depression, mood swings, or other mental health symptoms are often addressed during general medical consultations.
Causes:
- Infections: Bacterial, viral, or fungal infections can cause a range of symptoms, prompting individuals to seek medical attention.
- Inflammatory Conditions: Conditions characterized by chronic inflammation, such as autoimmune diseases or inflammatory disorders, may lead to a variety of symptoms.
- Chronic Diseases: Conditions like diabetes, hypertension, or cardiovascular diseases may require ongoing medical consultations for management and monitoring.
- Injuries: Traumatic injuries or accidents may necessitate medical consultations for proper assessment and treatment.
- Genetic Predisposition: Individuals with a family history of certain medical conditions may seek consultations for preventive care or early detection.
Types:
- Routine Check-up: Regular consultations for preventive healthcare, including screenings, vaccinations, and overall health assessments.
- Acute Illness Consultation: Seeking medical advice for sudden-onset symptoms or illnesses, such as infections, injuries, or respiratory issues.
- Chronic Disease Management: Ongoing consultations for individuals with chronic conditions, focusing on medication management, lifestyle adjustments, and monitoring.
- Preventive Care: Consultations focused on maintaining good health, discussing lifestyle choices, and addressing risk factors for potential health issues.
- Specialized Consultations: Referrals to specialists may be part of general medical consultations when specific expertise is required for diagnosis or treatment.
- Mental Health Consultation: Discussions about mental health concerns, including stress, anxiety, depression, or other psychological symptoms.
General medical consultations are essential for early detection of health issues, ongoing management of chronic conditions, and overall well-being. They provide an opportunity for patients to discuss their health concerns, receive guidance on preventive measures, and establish a partnership with healthcare professionals for optimal health outcomes. Regular consultations play a crucial role in maintaining overall health and addressing health concerns promptly and effectively.
Growth development disorders

Growth development disorders
Growth and development disorders encompass a range of conditions that affect a person’s physical growth and overall development. These disorders can manifest in childhood or later in life and may be influenced by genetic, environmental, or medical factors. Understanding the symptoms, causes, and types of growth and development disorders is crucial for diagnosis and appropriate management.
Symptoms:
Symptoms of growth and development disorders can vary widely depending on the specific disorder and its underlying causes. Common signs may include:
- Delayed Milestones: Delays in achieving developmental milestones, such as sitting up, crawling, walking, or speaking, may be indicative of a growth and development disorder.
- Short Stature: A child significantly shorter than peers of the same age may be experiencing a growth disorder.
- Cognitive Delays: Learning difficulties, intellectual disabilities, or challenges in academic performance may be associated with certain growth and development disorders.
- Facial Abnormalities: Some genetic disorders can cause distinctive facial features that indicate an underlying growth disorder.
- Delayed Puberty: In adolescents, delayed onset of puberty or slow progression through puberty stages may signal a growth disorder.
Causes:
- Genetic Factors: Many growth and development disorders have a genetic basis, resulting from mutations or abnormalities in genes that regulate growth.
- Chromosomal Abnormalities: Disorders such as Down syndrome, Turner syndrome, or Prader-Willi syndrome involve abnormalities in the number or structure of chromosomes.
- Hormonal Imbalances: Disorders affecting the endocrine system, such as growth hormone deficiency or thyroid disorders, can impact growth and development.
- Nutritional Deficiencies: Inadequate nutrition, including deficiencies in essential vitamins and minerals, can hinder proper growth.
- Chronic Illnesses: Certain chronic medical conditions, such as kidney disease or congenital heart defects, may affect growth and development.
- Environmental Factors: Exposure to toxins, infections, or other environmental factors during pregnancy or early childhood can contribute to growth and development disorders.
Types:
- Growth Hormone Deficiency: Insufficient production of growth hormone can lead to short stature and delayed development.
- Turner Syndrome: A chromosomal disorder affecting females, characterized by short stature and absence or underdevelopment of the ovaries.
- Prader-Willi Syndrome: A genetic disorder associated with intellectual disabilities, obesity, and growth hormone deficiency.
- Down Syndrome: Caused by an extra chromosome 21, Down syndrome is characterized by intellectual disabilities, distinct facial features, and potential growth delays.
- Russell-Silver Syndrome: A rare genetic disorder resulting in intrauterine and postnatal growth restriction, often with a proportionally small stature.
- Constitutional Growth Delay: A temporary delay in growth and development that usually corrects itself, often observed in children who catch up in height during adolescence.
Early intervention and a multidisciplinary approach involving healthcare professionals, educators, and support services are crucial for managing growth and development disorders effectively. Regular medical monitoring and individualized treatment plans can help optimize outcomes for individuals with these conditions.
Headache

Headache
A headache is a common condition characterized by pain or discomfort in the head or neck region. It can range from a mild annoyance to severe and debilitating pain, affecting daily activities. Understanding the symptoms, causes, and types of headaches is essential for effective management and relief.
Symptoms:
Headaches can present with various symptoms, and the specific features may vary depending on the type of headache. Common symptoms include:
- Pain: The most noticeable symptom is pain, which can be dull, throbbing, sharp, or pulsating.
- Location: The pain may be localized to a specific area of the head or neck, or it can be more generalized.
- Duration: Headaches can be brief and episodic or prolonged, lasting for hours or even days.
- Sensitivity to Light and Sound: Many individuals with headaches experience increased sensitivity to light (photophobia) or sound (phonophobia).
- Nausea and Vomiting: Some types of headaches, particularly migraines, can be accompanied by nausea and vomiting.
- Aura: Certain types of migraines may be preceded by an aura, which includes visual disturbances, sensory changes, or other neurological symptoms.
Causes:
- Tension: Tension-type headaches are often associated with stress, muscle tension, or poor posture.
- Migraines: Migraines are a type of primary headache characterized by moderate to severe pulsating pain, often accompanied by other symptoms like nausea and sensitivity to light.
- Cluster Headaches: These are severe headaches that occur in clusters, with multiple attacks over a period of weeks or months, separated by headache-free intervals.
- Sinus: Headaches associated with sinusitis or sinus infections can cause pain around the eyes, forehead, or cheeks.
- Rebound: Overuse of pain medications, especially those containing caffeine or codeine, can lead to rebound headaches.
- Hormonal: Hormonal fluctuations, particularly in women, can trigger headaches, such as menstrual migraines.
- Secondary Causes: Headaches can be a symptom of underlying medical conditions, including infections, head injuries, or vascular issues.
Types:
- Tension-Type Headaches: The most common type, characterized by a steady ache on both sides of the head.
- Migraines: Typically involve moderate to severe throbbing pain, often on one side of the head, and may be accompanied by aura, nausea, and sensitivity to light.
- Cluster Headaches: Intense, stabbing pain that occurs in clusters, often around the eye, and is associated with other symptoms like nasal congestion and tearing.
- Sinus Headaches: Pain around the forehead, cheeks, or eyes, often associated with sinus congestion or infections.
- Rebound Headaches: Result from overuse of pain medications, and the headaches often worsen when the medication wears off.
Insomnia (Sleeplessness)

Insomnia (Sleeplessness)
Insomnia: Unpacking Symptoms, Causes, and Types
Insomnia is a common sleep disorder characterized by difficulty falling asleep, staying asleep, or experiencing non-restorative sleep despite having the opportunity to sleep. This condition can significantly impact daily functioning, mood, and overall well-being. Understanding the symptoms, causes, and types of insomnia is crucial for effective management and improved sleep quality.
Symptoms:
- Difficulty Falling Asleep: Individuals with insomnia often struggle to initiate sleep, spending an extended period in bed before finally falling asleep.
- Frequent Awakenings: Insomnia may manifest as waking up multiple times during the night, disrupting the natural sleep cycle and impairing the ability to achieve deep, restful sleep.
- Early Morning Awakening: Some individuals with insomnia wake up earlier than desired and find it challenging to return to sleep, resulting in overall reduced sleep duration.
- Non-Restorative Sleep: Despite spending an adequate amount of time in bed, individuals with insomnia may wake up feeling unrefreshed and fatigued, leading to daytime sleepiness.
- Daytime Impairment: Insomnia can impact daily functioning, causing difficulties concentrating, irritability, mood disturbances, and impaired performance at work or school.
- Increased Anxiety About Sleep: Individuals with insomnia often develop heightened anxiety or worry about their ability to fall asleep, creating a cycle of sleep-related stress.
Causes:
- Stress and Anxiety: Elevated stress levels or persistent anxiety can contribute to difficulty falling asleep and maintaining restful sleep.
- Depression: Insomnia is commonly associated with depression. Sleep disturbances and changes in sleep architecture often accompany depressive disorders.
- Poor Sleep Hygiene: Irregular sleep schedules, excessive use of electronic devices before bedtime, or an uncomfortable sleep environment can disrupt the natural sleep-wake cycle.
- Medical Conditions: Various medical conditions, including chronic pain, respiratory disorders, or hormonal imbalances, can contribute to insomnia.
- Medications: Certain medications, such as stimulants, antidepressants, or medications that affect the circadian rhythm, may interfere with normal sleep patterns.
- Substance Use: Alcohol, nicotine, and caffeine can disrupt sleep and contribute to the development or exacerbation of insomnia.
- Shift Work: Irregular work schedules, especially night shifts, can disrupt the body’s natural circadian rhythm, leading to insomnia.
- Psychological Factors: Trauma, grief, or other psychological factors can contribute to insomnia, particularly when these issues are unresolved or cause ongoing distress.
- Age: Insomnia is more prevalent in older adults, often due to changes in sleep architecture, increased medical conditions, or medication use.
Types:
- Acute Insomnia: This type is brief and often occurs in response to a specific stressor or life event. Once the stressor is resolved or adaptation occurs, sleep typically returns to normal.
- Chronic Insomnia: Chronic insomnia involves persistent sleep difficulties lasting at least three nights per week for three months or longer. It can be related to various factors, including medical conditions, lifestyle, or underlying sleep disorders.
- Comorbid Insomnia: Insomnia may coexist with other medical or psychiatric conditions, such as depression or anxiety, leading to a more complex presentation that requires targeted treatment.
- Onset Insomnia: Onset insomnia refers to difficulty falling asleep at the beginning of the night, often taking an extended period to initiate sleep.
- Maintenance Insomnia: Maintenance insomnia involves difficulty staying asleep, with frequent awakenings during the night. Individuals may find it challenging to return to sleep after waking.
- Early Morning Awakening: Early morning awakening is characterized by waking up earlier than desired and being unable to return to sleep. This can result in decreased overall sleep duration.
- Behavioral Insomnia of Childhood: This type is specific to children and is characterized by difficulties falling asleep or staying asleep, often due to behavioral factors or parental responses to sleep-related behaviors.
In conclusion, insomnia is a complex sleep disorder with various symptoms, causes, and types. Successful management often involves a multifaceted approach, considering behavioral, psychological, and environmental factors. Seeking professional guidance is crucial for an accurate diagnosis and the development of a personalized treatment plan tailored to the specific needs of each individual experiencing insomnia.
Leg swelling

Leg swelling
Leg Swelling: Unraveling Symptoms, Causes, and Types
Leg swelling, also known as peripheral edema, is a condition characterized by the accumulation of fluid in the tissues of the legs. This swelling can range from mild to severe and may be a symptom of an underlying medical issue. Understanding the symptoms, causes, and types of leg swelling is crucial for proper diagnosis and management.
Symptoms:
- Visible Swelling: The primary symptom is the noticeable enlargement of one or both legs. Swelling can occur in the feet, ankles, calves, and thighs.
- Pitting Edema: When pressure is applied to the swollen area, a visible indentation or “pit” may remain for a few seconds. This is known as pitting edema and is commonly seen in conditions affecting fluid balance.
- Heaviness or Tightness: Individuals with leg swelling often report a sensation of heaviness or tightness in the affected limbs.
- Reduced Range of Motion: Severe leg swelling can limit the range of motion, making it difficult for individuals to move their legs comfortably.
- Discomfort or Pain: Swollen legs may be accompanied by discomfort or pain. The pain can range from a mild ache to sharp and throbbing sensations.
- Skin Changes: The skin over the swollen area may appear stretched, shiny, or have a puffy appearance. In some cases, the skin may feel warm to the touch.
- Difficulty Fitting into Shoes: Due to the swelling, individuals may find it challenging to fit into their regular shoes.
Causes:
- Fluid Retention: The most common cause of leg swelling is fluid retention, which can result from conditions affecting the balance of fluids in the body.
- Venous Insufficiency: When the veins in the legs fail to adequately pump blood back to the heart, fluid can accumulate in the tissues, leading to swelling. This condition is often associated with prolonged standing or sitting.
- Lymphedema: Lymphedema occurs when the lymphatic system, responsible for draining excess fluid from tissues, is impaired. This can lead to the accumulation of lymphatic fluid and subsequent leg swelling.
- Heart Failure: In heart failure, the heart is unable to pump blood effectively, leading to fluid buildup in various parts of the body, including the legs.
- Kidney Disease: Impaired kidney function can result in the retention of salt and water, contributing to fluid buildup and leg swelling.
- Liver Disease: Liver conditions, such as cirrhosis, can lead to decreased protein production, causing fluid to leak into the surrounding tissues and lead to swelling.
- Deep Vein Thrombosis (DVT): DVT is a blood clot that forms in a deep vein, often in the legs. This can obstruct blood flow and result in leg swelling.
- Peripheral Artery Disease (PAD): PAD can cause poor circulation, leading to swelling and discomfort in the legs.
- Infections: Infections affecting the legs, such as cellulitis, can cause inflammation and fluid buildup, resulting in swelling.
- Injuries or Trauma: Trauma or injuries to the legs can cause localized swelling due to inflammation and tissue damage.
Types:
- Peripheral Edema: Peripheral edema refers to swelling that occurs in the extremities, such as the legs, ankles, and feet. It is a common manifestation of fluid retention.
- Localized Edema: This type of swelling is confined to a specific area, often due to injury, infection, or inflammation in that particular region.
- Bilateral Edema: Bilateral leg swelling occurs in both legs and is commonly associated with systemic conditions such as heart failure, kidney disease, or liver disease.
- Unilateral Edema: Unilateral leg swelling affects only one leg and may be caused by conditions such as DVT, injury, or lymphedema in that specific limb.
- Pitting Edema: Pitting edema is characterized by the formation of a temporary pit or indentation when pressure is applied to the swollen area. It is commonly seen in conditions causing fluid retention.
- Non-Pitting Edema: In non-pitting edema, the swollen area does not leave a pit when pressure is applied. This type of edema is often associated with lymphatic issues, such as lymphedema.
- Cyclic Edema: Cyclic edema is characterized by periodic episodes of swelling that may be influenced by factors such as hormonal changes, weather, or prolonged standing.
- Inflammatory Edema: Inflammatory edema results from inflammation in the affected tissues and is often associated with conditions like arthritis or cellulitis.
Leg Ulcers

Leg Ulcers
Leg Ulcers: Unveiling Symptoms, Causes, and Types
Leg ulcers are open sores or wounds that develop on the lower extremities, typically below the knee. These ulcers can be chronic, persisting for an extended period, and may significantly impact an individual’s quality of life. Understanding the symptoms, causes, and types of leg ulcers is crucial for accurate diagnosis and effective management.
Symptoms:
- Open Sores: The hallmark symptom of leg ulcers is the presence of open sores or wounds on the skin of the lower legs. These ulcers may vary in size and depth.
- Pain: Leg ulcers can be associated with pain, ranging from mild discomfort to severe, throbbing pain. Pain levels may fluctuate based on the underlying cause and the stage of the ulcer.
- Itching: Itching or irritation around the ulcerated area is common and may contribute to the discomfort experienced by individuals with leg ulcers.
- Redness and Inflammation: The skin surrounding the ulcer may appear red and inflamed. Inflammation is often a response to the ongoing wound healing process.
- Swelling: Swelling, known as edema, may be present in the affected leg. This can result from impaired circulation or underlying venous insufficiency.
- Discharge: Leg ulcers may produce discharge, which can range from clear fluid to pus. The nature of the discharge may provide insights into the type of infection or wound characteristics.
- Odor: In some cases, leg ulcers can emit an unpleasant odor, especially if there is an infection present.
- Change in Skin Texture: The skin around the ulcer may undergo changes in texture, becoming hardened or discolored.
Causes:
- Venous Insufficiency: Chronic venous insufficiency, where the veins have difficulty returning blood to the heart, is a leading cause of leg ulcers. The pooling of blood in the legs can result in skin breakdown and ulcer formation.
- Arterial Insufficiency: Poor blood circulation due to arterial insufficiency can lead to inadequate oxygen and nutrient supply to the tissues, predisposing the legs to ulceration.
- Diabetes: Individuals with diabetes are at an increased risk of developing leg ulcers due to complications such as peripheral neuropathy and impaired wound healing.
- Pressure Ulcers: Prolonged pressure on a specific area, commonly occurring in bedridden or wheelchair-bound individuals, can cause pressure ulcers that may progress to open sores.
- Peripheral Artery Disease (PAD): PAD restricts blood flow to the legs, increasing the risk of ulcers, particularly on the toes or feet.
- Trauma or Injury: Physical trauma, such as cuts, burns, or fractures, can lead to open wounds that may develop into ulcers if not properly treated.
- Infection: Infections, whether bacterial, viral, or fungal, can contribute to the development and worsening of leg ulcers.
- Autoimmune Diseases: Conditions like rheumatoid arthritis or lupus can affect the skin, increasing susceptibility to ulcer formation.
- Deep Vein Thrombosis (DVT): Blood clots in the deep veins of the legs can lead to venous congestion, increasing the risk of ulcers.
- Obesity: Excess weight can put additional pressure on the lower extremities, contributing to venous insufficiency and increasing the risk of leg ulcers.
Types:
- Venous Ulcers: These are the most common type of leg ulcers and typically occur due to chronic venous insufficiency. Venous ulcers often develop on the inner side of the leg, above the ankle.
- Arterial Ulcers: Arterial ulcers result from inadequate blood supply to the legs, commonly associated with conditions like peripheral artery disease. These ulcers often occur on the feet, toes, or lower leg.
- Neuropathic Ulcers: Individuals with diabetes often experience neuropathy, leading to reduced sensation in the feet. Neuropathic ulcers can result from minor injuries or pressure, often on the sole of the foot.
- Pressure Ulcers: Also known as bedsores or decubitus ulcers, pressure ulcers develop due to prolonged pressure on a specific area of the skin. They commonly occur over bony prominences in bedridden individuals.
- Mixed Ulcers: In some cases, leg ulcers may have a combination of causes, such as both venous and arterial insufficiency contributing to ulcer formation.
- Traumatic Ulcers: Ulcers resulting from injuries, burns, or other forms of trauma fall into this category. Proper wound care is essential to prevent infection and facilitate healing.
- Infectious Ulcers: Ulcers caused by infections, whether bacterial, viral, or fungal, can lead to tissue breakdown and the formation of open sores.
- Autoimmune Ulcers: In individuals with autoimmune diseases, skin involvement can lead to the development of ulcers. Conditions like vasculitis or lupus may contribute to autoimmune-related ulcers.
Malabsorption

Malabsorption
Understanding Malabsorption: Symptoms, Causes, and Types
Malabsorption is a digestive disorder characterized by the inadequate absorption of nutrients from the gastrointestinal tract into the bloodstream. This condition can result from various underlying causes, leading to a range of symptoms and nutritional deficiencies. Understanding malabsorption involves recognizing its symptoms, exploring potential causes, and identifying different types of this digestive disorder.
Symptoms:
- Diarrhoea:
– Chronic or recurrent diarrhoea is a common symptom of malabsorption. It occurs due to the inefficient absorption of nutrients and excess water in the intestines.
- Weight Loss:
– Inadequate absorption of essential nutrients can lead to weight loss, malnutrition, and a general lack of energy.
- Steatorrhea:
– Fatty, greasy stools (steatorrhea) result from the poor absorption of fats. Stools may appear pale and float in water.
- Abdominal Pain and Bloating:
– Abdominal discomfort, pain, and bloating can occur due to the malabsorption-induced changes in the gastrointestinal tract.
- Weakness and Fatigue:
– Malabsorption often leads to nutrient deficiencies, causing weakness, fatigue, and an overall sense of lethargy.
- Nutrient Deficiencies:
– Deficiencies in vitamins (especially fat-soluble vitamins like A, D, E, and K), minerals, and other essential nutrients can manifest as various symptoms, such as bruising (vitamin K deficiency) or bone pain (vitamin D deficiency).
- Anaemia:
– Malabsorption may lead to anaemia due to deficiencies in iron, vitamin B12, or folate.
- Edema:
– Protein malabsorption can result in edema (swelling) due to a lack of proteins to maintain fluid balance.
Causes:
- Celiac Disease:
– An autoimmune condition where the ingestion of gluten leads to damage in the small intestine, impairing nutrient absorption.
- Crohn’s Disease:
– An inflammatory bowel disease causing inflammation anywhere in the digestive tract, leading to malabsorption.
- Pancreatic Insufficiency:
– Conditions such as chronic pancreatitis or cystic fibrosis can reduce pancreatic enzyme production, affecting fat digestion.
- Bile Salt Deficiency:
– Diseases affecting the liver or gallbladder can result in insufficient bile production, affecting fat absorption.
- Small Intestinal Bacterial Overgrowth (SIBO):
– Abnormal growth of bacteria in the small intestine can interfere with nutrient absorption.
- Short Bowel Syndrome:
– Surgical removal of a significant portion of the small intestine due to conditions like Crohn’s disease or injuries can lead to malabsorption.
- Parasitic Infections:
– Infections caused by parasites, such as Giardia lamblia, can disrupt the normal absorption processes in the intestines.
- Whipple’s Disease:
– A rare bacterial infection affecting the small intestine, causing malabsorption.
Types of Malabsorption:
- Lactose Malabsorption:
– Inability to digest lactose, a sugar found in milk and dairy products, due to insufficient lactase enzyme production.
- Fat Malabsorption (Steatorrhea):
– Inefficient absorption of fats leads to fatty, greasy stools. Conditions like pancreatic insufficiency or bile salt deficiency contribute to fat malabsorption.
- Protein Malabsorption:
– Insufficient absorption of proteins, leading to deficiencies and related symptoms such as edema and muscle wasting.
- Vitamin Malabsorption:
– Deficiencies in fat-soluble vitamins (A, D, E, K) or water-soluble vitamins (B12, folate) due to impaired absorption processes.
- Mineral Malabsorption:
– Poor absorption of essential minerals, including iron, calcium, magnesium, and zinc, leading to various deficiencies.
- Selective Nutrient Malabsorption:
– Specific nutrients, such as certain amino acids or carbohydrates, may not be absorbed properly, resulting in deficiencies.
Understanding malabsorption involves a comprehensive approach, combining diagnostic measures, nutritional interventions, and targeted treatments for underlying causes. Timely diagnosis and proper management are crucial for improving symptoms, preventing complications, and promoting overall health. Individuals experiencing persistent gastrointestinal symptoms or unexplained nutritional deficiencies should seek medical evaluation for an accurate diagnosis and tailored treatment plan.
Migraine

Migraine
Migraine: Unraveling Symptoms, Causes, and Types
Migraine is a neurological disorder characterized by recurring, severe headaches that are often accompanied by other symptoms such as nausea, vomiting, and sensitivity to light and sound. It can significantly impact an individual’s daily life, and understanding the symptoms, causes, and types of migraines is crucial for effective management and relief.
Symptoms:
- Intense Headache: The hallmark symptom of a migraine is a throbbing or pulsating headache, often on one side of the head. The pain is usually moderate to severe and can hinder daily activities.
- Sensitivity to Light (Photophobia): Many individuals with migraines experience sensitivity to light, making bright lights or sunlight uncomfortable during an attack.
- Sensitivity to Sound (Phonophobia): Loud noises or certain sounds can exacerbate migraine symptoms. Phonophobia is common during migraine attacks.
- Nausea and Vomiting: Migraine attacks often come with nausea, and some individuals may vomit during or after the headache phase.
- Aura: A subset of migraines, known as migraine with aura, involves visual or sensory disturbances that precede or accompany the headache. Auras can include flashing lights, zigzag lines, or temporary vision loss.
- Visual Disturbances: In addition to auras, migraines can cause other visual disturbances, such as seeing spots or experiencing blurred vision.
- Aura without Headache: Some individuals may experience an aura without the subsequent headache. This is known as a “silent” or “acephalic” migraine.
- Dizziness and Vertigo: Migraines can be associated with feelings of dizziness or vertigo, impacting balance and coordination.
- Tingling or Numbness: Some individuals may experience tingling or numbness in the face or limbs, known as the sensory aura.
Causes:
- Genetic Predisposition: There is a strong genetic component to migraines. If a family member experiences migraines, an individual may be more susceptible to developing them.
- Abnormal Brain Activity: Migraines are believed to involve abnormal brain activity, particularly changes in the neurotransmitters serotonin and dopamine. These changes can affect blood vessels and lead to the characteristic symptoms.
- Triggers: Various factors can trigger migraines in susceptible individuals. Common triggers include certain foods (chocolate, caffeine, aged cheese), hormonal changes (menstruation, pregnancy), stress, lack of sleep, environmental factors (bright lights, strong odors), and changes in weather.
- Hormonal Changes: Hormonal fluctuations, especially in women, can contribute to migraines. Many women experience migraines related to their menstrual cycles.
- Neurological Factors: Migraines are considered a neurological disorder, and abnormalities in the brainstem and its interaction with the trigeminal nerve may play a role in migraine development.
- Vascular Changes: Changes in blood flow and dilation of blood vessels in the brain are associated with migraines. The exact relationship between vascular changes and migraines is complex and not fully understood.
Types:
- Migraine without Aura (Common Migraine):
– Symptoms: Throbbing headache, often one-sided, accompanied by nausea, vomiting, and sensitivity to light and sound.
– Duration: Can last from a few hours to several days.
- Migraine with Aura (Classic Migraine):
– Symptoms: Preceded or accompanied by visual or sensory disturbances known as auras. Auras can include flashing lights, zigzag lines, or temporary vision loss.
– Duration: Auras typically last for less than an hour, followed by the headache phase.
- Chronic Migraine:
– Frequency: Occurs on 15 or more days per month for at least three months, with features of a migraine headache on at least eight days.
- Menstrual Migraine:
– Trigger: Typically occurs in relation to the menstrual cycle, often just before, during, or after menstruation.
– Symptoms: Similar to other migraines, but the timing is linked to hormonal changes.
- Vestibular Migraine:
– Symptoms: Characterized by vertigo, dizziness, and balance issues, often without the classic headache.
– Duration: Episodes may last minutes to hours.
- Ocular Migraine (Retinal Migraine):
– Symptoms: Temporary vision loss or blindness in one eye, often accompanied by a headache.
– Duration: Vision loss typically resolves within an hour.
- Status Migrainosus:
– Duration: An exceptionally long and severe migraine attack lasting for more than 72 hours, sometimes requiring medical intervention.
- Silent Migraine (Aura without Headache):
– Symptoms: Experience an aura without the subsequent headache phase.
– Duration: The aura phase may last less than an hour.
Mouth Ulcers (Apthous Ulcers)

Mouth Ulcers (Apthous Ulcers)
Mouth Ulcers: Unraveling Symptoms, Causes, and Types
Mouth ulcers, also known as canker sores or aphthous ulcers, are painful sores that develop on the mucous membranes inside the mouth. While they are generally harmless and not contagious, mouth ulcers can cause discomfort and difficulty eating or speaking. Understanding the symptoms, causes, and types of mouth ulcers is essential for effective management and relief.
Symptoms:
- Painful Sores: The primary symptom of mouth ulcers is the presence of painful sores or lesions in the mouth. These sores can vary in size and shape.
- Round or Oval Shape: Most mouth ulcers have a round or oval shape with a white or yellowish center and a red border. The appearance can be similar to a small, shallow crater.
- Redness and Inflammation: The area surrounding the ulcer may be red and inflamed. In severe cases, the inflammation can extend beyond the immediate vicinity of the sore.
- Burning Sensation: Individuals with mouth ulcers often experience a burning or tingling sensation before the sores become visible.
- Discomfort while Eating or Drinking: The presence of mouth ulcers can make eating and drinking painful, especially when these activities involve contact with the affected area.
- Difficulty Speaking: Depending on the location of the ulcers, individuals may experience difficulty speaking, particularly if the sores come into contact with the tongue or other oral structures.
- Recurrent Episodes: Mouth ulcers can recur periodically, with some individuals experiencing multiple episodes throughout the year.
Causes:
- Minor Trauma or Injury: Minor trauma or injury to the soft tissues inside the mouth, such as accidental bites, dental work, or irritation from braces or dentures, can contribute to the development of mouth ulcers.
- Stress and Anxiety: Emotional stress and anxiety are known triggers for mouth ulcers. The exact mechanisms linking stress to ulcer formation are not fully understood but may involve the immune response.
- Hormonal Changes: Some individuals, particularly women, may experience mouth ulcers during hormonal changes, such as menstruation or pregnancy.
- Dietary Factors: Certain dietary factors, such as consuming acidic or spicy foods, can contribute to the development of mouth ulcers in susceptible individuals.
- Nutritional Deficiencies: Deficiencies in essential nutrients, including vitamin B12, iron, folic acid, and zinc, can increase the risk of mouth ulcers.
- Immune System Dysfunction: Conditions that affect the immune system, such as autoimmune disorders, may be associated with an increased likelihood of developing mouth ulcers.
- Genetic Predisposition: There may be a genetic component to susceptibility to mouth ulcers, as individuals with a family history of recurrent ulcers may be more prone to developing them.
- Infections: In some cases, infections, such as viral or bacterial infections, can contribute to the formation of mouth ulcers.
Types:
- Minor Aphthous Ulcers:
– Size: These are the most common type and are typically small, measuring less than 1 centimeter in diameter.
– Healing Time: Minor ulcers usually heal within one to two weeks without scarring.
- Major Aphthous Ulcers:
– Size: Major ulcers are larger than minor ones, often exceeding 1 centimeter in diameter.
– Healing Time: Healing may take several weeks, and scarring is more likely.
- Herpetiform Aphthous Ulcers:
– Size: Despite the name, herpetiform ulcers are not related to the herpes virus. They are small, pinpoint-sized ulcers that often cluster together.
– Number: Numerous herpetiform ulcers can develop in a single outbreak.
– Healing Time: Like minor ulcers, herpetiform ulcers usually heal without scarring.
Oral thrush
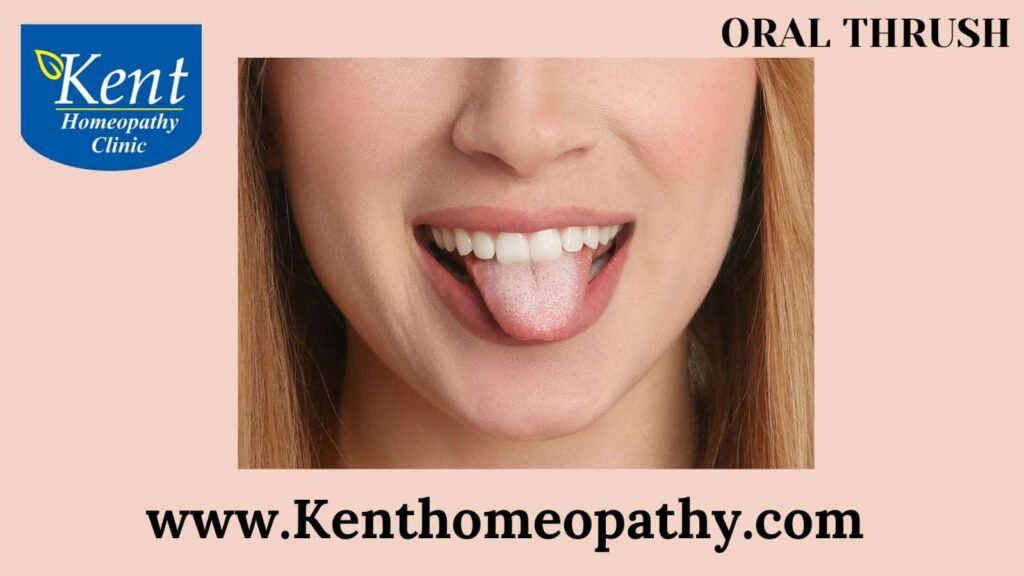
Oral thrush
Oral Thrush: Unveiling Symptoms, Causes, and Types
Oral thrush, also known as oropharyngeal candidiasis, is a fungal infection caused by Candida albicans. This condition primarily affects the mouth and throat, leading to the development of white, creamy lesions on the tongue, inner cheeks, and other areas of the oral cavity. Understanding the symptoms, causes, and types of oral thrush is crucial for accurate diagnosis and effective management.
Symptoms:
- White Lesions:
– The hallmark symptom of oral thrush is the presence of white or creamy lesions on the tongue, inner cheeks, roof of the mouth, and sometimes the back of the throat.
– These lesions may resemble cottage cheese and can be easily scraped off, revealing red and sometimes bleeding tissue underneath.
- Pain and Discomfort:
– Individuals with oral thrush may experience pain or discomfort while eating or swallowing.
– The affected areas may be sensitive to touch and can cause a burning sensation.
- Redness and Inflammation:
– The surrounding areas of the white lesions may appear red and inflamed.
– In severe cases, cracks or small sores may develop at the corners of the mouth.
- Loss of Taste:
– The presence of oral thrush can lead to a temporary loss of taste or altered taste perception.
- Cottony Feeling in the Mouth:
– Some individuals may describe a cottony or dry feeling in the mouth, contributing to a sense of discomfort.
- Difficulty Swallowing:
– Severe cases of oral thrush may lead to difficulty swallowing, especially if the lesions extend to the back of the throat.
- Unpleasant Breath:
– Oral thrush can contribute to bad breath or an unpleasant taste in the mouth.
Causes:
- Candida Overgrowth:
– Oral thrush is primarily caused by an overgrowth of Candida albicans, a type of yeast that normally resides in the mouth in small amounts.
– Factors such as a weakened immune system, certain medications, or hormonal changes can contribute to the proliferation of Candida.
- Weakened Immune System:
– Conditions that weaken the immune system, such as HIV/AIDS, chemotherapy, or immunosuppressive medications, increase the risk of oral thrush.
- Antibiotic Use:
– Antibiotics can disrupt the balance of microorganisms in the mouth, leading to an overgrowth of Candida.
- Denture Use:
– Ill-fitting dentures or poor oral hygiene in individuals who wear dentures can create an environment conducive to Candida overgrowth.
- Medical Conditions:
– Conditions like diabetes, dry mouth (xerostomia), and autoimmune disorders may increase susceptibility to oral thrush.
- Hormonal Changes:
– Hormonal changes, such as those occurring during pregnancy or in individuals taking oral contraceptives, can alter the oral environment, contributing to Candida overgrowth.
- Smoking:
– Smoking can impair the function of the immune system and create an environment favorable for fungal infections.
Types:
- Pseudomembranous Candidiasis:
– Description: Characterized by white, curd-like patches on the tongue, inner cheeks, and other oral surfaces.
– Scraping: Lesions can be easily scraped off, revealing red or bleeding tissue underneath.
– Common Cause: Weakened immune system, antibiotic use.
- Erythematous Candidiasis:
– Description: Presents as red, flat lesions on the tongue and palate.
– Common Cause: Immunocompromised individuals, antibiotic use, denture wearers.
- Hyperplastic Candidiasis:
– Description: Characterized by persistent white lesions that cannot be easily scraped off.
– Common Cause: Chronic Candida infections, immunocompromised individuals.
- Angular Cheilitis:
– Description: Involves red, swollen sores at the corners of the mouth.
– Common Cause: Candida overgrowth, often seen in individuals with ill-fitting dentures.
Poor Appetite

Poor Appetite
Poor Appetite: Understanding Symptoms, Causes, and Types
Poor appetite, clinically referred to as anorexia, is a condition characterized by a reduced desire or interest in eating. While it’s common for appetite to fluctuate based on factors like stress or illness, persistent and unexplained loss of appetite can be a concerning health issue. Understanding the symptoms, causes, and types of poor appetite is crucial for effective management.
Symptoms:
- Reduced Food Intake:
– The primary symptom is a noticeable decrease in the amount of food an individual consumes compared to their usual eating habits.
- Weight Loss:
– Persistent poor appetite often leads to unintentional weight loss, as the body is not receiving sufficient nutrients.
- Fatigue:
– Inadequate nutrition can result in fatigue and a lack of energy, affecting daily activities.
- Nutrient Deficiency:
– Poor appetite may contribute to nutritional deficiencies, impacting overall health and potentially leading to other health issues.
- Changes in Taste Preferences:
– Individuals with poor appetite may experience alterations in taste preferences or find food less appealing.
- Digestive Issues:
– Constipation, indigestion, or other digestive problems can accompany poor appetite.
- Emotional Changes:
– Feelings of irritability, mood swings, or changes in emotional well-being may be associated with poor appetite.
Causes:
- Underlying Medical Conditions:
– Various medical conditions can lead to poor appetite, including chronic illnesses like cancer, kidney disease, liver disease, and infections.
- Mental Health Disorders:
– Conditions such as depression, anxiety, and eating disorders like anorexia nervosa can significantly impact appetite.
- Medications:
– Certain medications, such as chemotherapy drugs, antibiotics, or medications that affect the central nervous system, may cause a loss of appetite.
- Gastrointestinal Issues:
– Disorders like gastritis, peptic ulcers, or gastroesophageal reflux disease (GERD) can contribute to poor appetite due to discomfort during eating.
- Hormonal Changes:
– Hormonal imbalances, particularly thyroid disorders or changes in sex hormones, can affect appetite.
- Age-related Factors:
– Aging can lead to changes in taste perception and a decrease in appetite, affecting nutritional intake in older individuals.
- Chronic Pain:
– Persistent pain can suppress appetite, making it challenging for individuals with chronic pain conditions to maintain a regular eating pattern.
Types:
- Acute Poor Appetite:
– Often a response to an immediate illness, infection, or stress, acute poor appetite is typically short-term and resolves as the underlying cause is addressed.
- Chronic Poor Appetite:
– When poor appetite persists over an extended period, it may be indicative of a chronic condition, such as a long-term illness or mental health disorder.
- Medication-induced Poor Appetite:
– Some medications, especially those with side effects affecting the gastrointestinal system or central nervous system, can lead to a diminished desire to eat.
- Psychological Poor Appetite:
– Associated with mental health conditions, psychological poor appetite is often linked to mood disorders or eating disorders.
- Physical Poor Appetite:
– Resulting from physical health issues, this type is commonly seen in conditions affecting the digestive system, hormones, or other physiological functions.
- Age-related Poor Appetite:
– Seen predominantly in older individuals, age-related poor appetite can be influenced by factors such as changes in taste perception and decreased physical activity.
Conclusion:
Poor appetite is a multifaceted condition with diverse causes and manifestations. Recognizing the symptoms, understanding potential underlying factors, and seeking timely medical evaluation are essential steps in addressing this concern. Tailored treatment approaches, including lifestyle modifications, medication adjustments, and psychological support, can significantly improve appetite and overall well-being. If you or someone you know is experiencing persistent poor appetite, consulting with healthcare professionals is paramount for accurate diagnosis and appropriate intervention.
Flatulence

Flatulence
Flatulence, commonly known as passing gas or farting, is a natural and normal part of the digestive process. It involves the release of gas accumulated in the digestive system through the rectum. While it’s a common bodily function, excessive or foul-smelling flatulence can be a source of discomfort and may indicate underlying digestive issues.
Symptoms:
- Passing Gas: The primary symptom of flatulence is the release of gas from the rectum, which can occur voluntarily or involuntarily.
- Abdominal Discomfort: Some individuals may experience bloating, distension, or mild abdominal discomfort associated with gas accumulation.
- Belching: While belching primarily involves the release of gas from the stomach through the mouth, it is related to the overall process of gas in the digestive system.
Causes:
- Normal Digestive Process: Flatulence is a natural byproduct of digestion. When bacteria in the colon break down undigested food, gases like carbon dioxide, methane, and hydrogen are produced.
- Dietary Factors:
– Gas-Producing Foods: Certain foods are known to produce more gas, including beans, lentils, cruciferous vegetables (broccoli, cabbage), onions, and carbonated drinks.
– High-Fiber Diet: While essential for digestive health, a sudden increase in fiber intake can initially lead to increased gas production.
– Artificial Sweeteners: Some sweeteners, particularly those ending in -ol (sorbitol, xylitol), can cause increased gas.
- Swallowing Air: Ingesting air while eating, drinking, or talking can contribute to gas in the digestive system.
- Gastrointestinal Conditions:
– Irritable Bowel Syndrome (IBS): Individuals with IBS may experience increased sensitivity to gas in the intestines.
– Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis can affect the digestive tract and lead to increased gas.
Types:
- Normal Flatulence: Occurs as a result of the normal digestive process and is not excessive or associated with significant discomfort.
- Excessive Flatulence: Some individuals may produce larger amounts of gas than others, leading to increased frequency of flatulence.
- Foul-Smelling Flatulence: The presence of foul-smelling gas may be related to the breakdown of certain foods in the colon or the composition of the gut microbiota.
While flatulence is a normal bodily function, persistent or severe symptoms should be evaluated by a healthcare professional. Understanding dietary triggers and making lifestyle adjustments can often help manage and reduce excessive flatulence.
Post Herpetic Neuralgia

Post Herpetic Neuralgia
Postherpetic Neuralgia: Understanding Symptoms, Causes, and Types:
Postherpetic neuralgia (PHN) is a painful condition that can develop after an episode of shingles, a viral infection caused by the varicella-zoster virus—the same virus responsible for chickenpox. PHN is characterized by persistent, often severe, pain in the areas where the shingles rash occurred. Understanding the symptoms, causes, and types of postherpetic neuralgia is crucial for managing and alleviating the associated discomfort.
Symptoms:
- Persistent Pain:
– The hallmark symptom of postherpetic neuralgia is prolonged pain in the affected area following the resolution of the shingles rash. The pain can be burning, stabbing, or throbbing in nature.
- Hypersensitivity:
– The affected skin may become extremely sensitive to touch, even to the point where clothing or a gentle breeze can trigger pain.
- Itching and Tingling:
– Sensations of itching or tingling may persist in the region affected by shingles.
- Numbness or Weakness:
– Some individuals may experience numbness or weakness in the affected area, adding to the overall discomfort.
- Sleep Disturbances:
– Chronic pain can interfere with sleep, leading to fatigue and exacerbating the impact on daily life.
- Emotional Distress:
– Living with persistent pain can contribute to emotional distress, including anxiety and depression.
Causes:
- Varicella-Zoster Virus Reactivation:
– Postherpetic neuralgia arises as a complication of shingles, which occurs when the varicella-zoster virus reactivates. After an initial chickenpox infection, the virus remains dormant in nerve cells and can re-emerge later in life, causing shingles.
- Age:
– The risk of developing postherpetic neuralgia increases with age, particularly in individuals over 60.
- Severity of Shingles:
– The risk of developing PHN is higher in cases where the shingles rash is severe or widespread.
- Weakened Immune System:
– Individuals with compromised immune systems, whether due to age, medical conditions, or medications, are at a higher risk.
- Genetic Factors:
– Some individuals may have a genetic predisposition that makes them more susceptible to developing postherpetic neuralgia.
- Pain Perception:
– Individual pain perception and the body’s response to nerve damage play a role in the development and severity of PHN.
Types:
- Classic Postherpetic Neuralgia:
– The most common type, characterized by persistent pain in the area where the shingles rash occurred. The pain can last for weeks to months after the rash has healed.
- Trigeminal Neuralgia:
– When shingles affect the trigeminal nerve, which is responsible for facial sensation, individuals may experience severe, stabbing pain in the face. This form can be particularly challenging due to its impact on facial functions like eating and talking.
- Ophthalmic Postherpetic Neuralgia:
– Involves pain in the eye area and is associated with shingles affecting the ophthalmic nerve. This type can lead to complications like vision problems and requires specialized management.
- Cranial Neuralgia:
– Occurs when shingles affect nerves in the head, leading to persistent pain and discomfort in the cranial region.
- Multiple Nerve Postherpetic Neuralgia:
– Some individuals may experience PHN that affects multiple nerves, leading to a broader area of persistent pain and discomfort.
In conclusion, postherpetic neuralgia is a challenging condition characterized by persistent pain following a shingles episode. Timely diagnosis, appropriate treatment, and preventive measures are crucial for managing symptoms and improving the overall well-being of individuals affected by this condition. If you suspect postherpetic neuralgia, seeking medical advice is essential for an accurate diagnosis and tailored treatment plan.
Sleep Apnea Syndrome

Sleep Apnea Syndrome
Sleep Apnea Disorder: Unraveling Symptoms, Causes, and Types
Sleep apnea is a sleep disorder characterized by pauses in breathing during sleep. These interruptions, known as apneas, can occur multiple times throughout the night, leading to disruptions in sleep patterns and potential health complications. Understanding the symptoms, causes, and types of sleep apnea is crucial for proper diagnosis and effective management.
Symptoms:
- Loud Snoring:
– One of the most common symptoms of sleep apnea is loud and persistent snoring. This occurs as a result of the narrowed or obstructed airway during sleep.
- Pauses in Breathing:
– Witnessed pauses in breathing during sleep are a hallmark sign. These pauses can last for a few seconds to a minute and may be followed by a snort or gasp as breathing resumes.
- Excessive Daytime Sleepiness:
– Individuals with sleep apnea often experience excessive daytime sleepiness, leading to drowsiness, difficulty staying awake, and decreased alertness.
- Morning Headaches:
– Morning headaches are a common complaint among those with sleep apnea, possibly due to the effects of oxygen deprivation during the night.
- Difficulty Concentrating:
– Impaired cognitive function, difficulty concentrating, and memory problems are associated with sleep apnea-related sleep disturbances.
- Irritability and Mood Changes:
– Sleep apnea can contribute to irritability, mood swings, and increased susceptibility to stress.
- Dry Mouth or Sore Throat:
– Breathing through the mouth, common in individuals with sleep apnea, can lead to a dry mouth or sore throat upon waking.
- Insomnia:
– Some individuals with sleep apnea experience difficulty falling asleep or staying asleep, contributing to insomnia.
Causes:
- Obstructive Sleep Apnea (OSA):
– OSA is the most prevalent form of sleep apnea and occurs when the muscles in the throat relax excessively, causing a partial or complete blockage of the airway.
- Central Sleep Apnea (CSA):
– CSA is less common and results from a failure of the brain to send proper signals to the muscles responsible for breathing.
- Complex or Mixed Sleep Apnea:
– Some individuals may have a combination of both obstructive and central sleep apnea, referred to as complex or mixed sleep apnea.
- Risk Factors:
– Various factors increase the risk of developing sleep apnea, including obesity, family history, being male, having a large neck circumference, being older, and having certain medical conditions like hypertension.
- Alcohol and Sedative Use:
– Consuming alcohol or sedatives before bedtime can relax the muscles in the throat, increasing the likelihood of airway obstruction.
- Smoking:
– Smoking contributes to inflammation and fluid retention in the airway, making it more susceptible to blockage.
- Nasal Congestion:
– Conditions that cause nasal congestion or obstruction, such as allergies or anatomical issues, can contribute to sleep apnea.
Types:
- Obstructive Sleep Apnea (OSA):
– OSA, the most prevalent type, occurs when the muscles at the back of the throat relax excessively, leading to airway obstruction.
- Central Sleep Apnea (CSA):
– CSA results from a failure of the brain to send appropriate signals to the muscles that control breathing.
- Complex Sleep Apnea Syndrome (Treatment-Emergent CSA):
– Complex sleep apnea, also known as treatment-emergent central sleep apnea, involves a combination of both obstructive and central sleep apnea. It may develop in individuals undergoing continuous positive airway pressure (CPAP) therapy for OSA.
Sleep disorders

Sleep disorders
Sleep Disorders: Unraveling Symptoms, Causes, and Types
Sleep disorders are a group of conditions that affect the quality, duration, and patterns of sleep. These disorders can lead to disruptions in the normal sleep-wake cycle, causing various physical, mental, and emotional consequences. Understanding the symptoms, causes, and types of sleep disorders is essential for proper diagnosis and effective management.
Symptoms:
- Insomnia:
– Persistent difficulty falling asleep, staying asleep, or experiencing non-restorative sleep characterizes insomnia. Individuals may feel fatigued, irritable, and have difficulty concentrating during waking hours.
- Excessive Daytime Sleepiness:
– Excessive daytime sleepiness (EDS) is a common symptom across several sleep disorders. It involves an overwhelming desire to sleep during waking hours, potentially leading to impaired functioning.
- Snoring:
– While snoring is common, loud and persistent snoring, especially accompanied by gasping or choking sounds, may indicate sleep apnea, a specific sleep disorder.
- Sleep Apnea:
– Sleep apnea is characterized by pauses in breathing during sleep, often accompanied by loud snoring and gasping for breath upon awakening. This can lead to disrupted sleep and daytime fatigue.
- Restless Legs Syndrome (RLS):
– RLS is characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations. Symptoms typically worsen at night and can interfere with falling asleep.
- Narcolepsy:
– Narcolepsy involves excessive daytime sleepiness and sudden, uncontrollable episodes of falling asleep during activities. Individuals with narcolepsy may also experience cataplexy, a sudden loss of muscle tone triggered by emotions.
- Nightmares and Night Terrors:
– Frequent and distressing nightmares or night terrors can disrupt sleep and lead to anxiety about going to bed.
- Sleepwalking (Somnambulism):
– Sleepwalking involves performing complex activities during sleep, such as walking or eating, without conscious awareness. Episodes can be brief or prolonged.
Causes:
- Genetic Factors:
– Some sleep disorders have a genetic component, making individuals more susceptible if there is a family history of sleep-related issues.
- Medical Conditions:
– Underlying medical conditions, such as chronic pain, respiratory disorders, or neurological disorders, can contribute to sleep disturbances.
- Mental Health Disorders:
– Anxiety, depression, and other mental health conditions can impact sleep quality and contribute to insomnia or other sleep disorders.
- Hormonal Changes:
– Hormonal fluctuations, such as those occurring during pregnancy, menopause, or certain endocrine disorders, can affect sleep patterns.
- Environmental Factors:
– Disruptions in the sleep environment, such as excessive noise, light, or uncomfortable temperatures, can contribute to sleep disturbances.
- Substance Use:
– Certain substances, including caffeine, nicotine, and certain medications, can interfere with sleep. Substance abuse, including alcohol and illicit drugs, can also contribute to sleep disorders.
- Shift Work and Irregular Schedules:
– Individuals working irregular hours or night shifts may experience circadian rhythm disruptions, leading to sleep disorders.
- Age-Related Changes:
– Aging can affect sleep patterns, with older adults often experiencing changes in sleep architecture and increased likelihood of sleep disorders.
Types:
- Insomnia Disorders:
– Insomnia disorders involve persistent difficulty falling asleep, staying asleep, or experiencing restorative sleep. Chronic insomnia can significantly impact daily functioning.
- Sleep Apnea:
– Sleep apnea is characterized by repeated pauses in breathing during sleep, leading to fragmented sleep and daytime fatigue. Obstructive sleep apnea (OSA) involves a physical blockage of the airway, while central sleep apnea (CSA) results from a failure of the brain to send proper signals for breathing.
- Restless Legs Syndrome (RLS):
– RLS is characterized by an urge to move the legs, often accompanied by uncomfortable sensations. Symptoms typically worsen at night and can disrupt sleep.
- Narcolepsy:
– Narcolepsy involves excessive daytime sleepiness and sudden, uncontrollable episodes of falling asleep during activities. Cataplexy, a sudden loss of muscle tone, is a common symptom.
- Parasomnias:
– Parasomnias include abnormal behaviors during sleep, such as sleepwalking, night terrors, or sleep-related eating disorder.
- Circadian Rhythm Sleep Disorders:
– Circadian rhythm sleep disorders involve disruptions in the body’s natural sleep-wake cycle. Conditions like shift work disorder or jet lag fall into this category.
- Hypersomnia Disorders:
– Hypersomnia disorders involve excessive daytime sleepiness despite getting adequate nighttime sleep. Conditions like idiopathic hypersomnia or recurrent hypersomnia are examples.
- Sleep-related Movement Disorders:
– Disorders like periodic limb movement disorder (PLMD) or restless legs syndrome (RLS) involve involuntary movements during sleep, impacting sleep quality.
Tumors

Tumors
Tumor: Understanding Symptoms, Causes, and Type
A tumor refers to an abnormal mass or lump of tissue that develops when cells divide and grow uncontrollably. Tumors can be either benign or malignant, and understanding their symptoms, causes, and types is crucial for accurate diagnosis and appropriate management.
Symptoms:
- Lump or Mass:
– The most common symptom of a tumor is the presence of a palpable lump or mass. Depending on the location and size of the tumor, it may or may not be noticeable externally.
- Changes in Size or Shape:
– Tumors can cause changes in the size, shape, or contours of the affected body part. This can be observed in organs or tissues where the tumor is growing.
- Pain or Discomfort:
– Pain or discomfort may occur if the tumor puts pressure on surrounding nerves, tissues, or organs. However, not all tumors cause pain, especially in the early stages.
- Changes in Skin Color or Texture:
– Skin overlying a tumor may show changes in color, texture, or temperature. This can include redness, warmth, or discoloration.
- Changes in Bowel or Bladder Habits:
– Tumors affecting the digestive or urinary systems may cause changes in bowel or bladder habits, such as blood in stool or urine, constipation, or increased frequency of urination.
- Unexplained Weight Loss:
– Unexplained weight loss can be a symptom of certain malignant tumors. This may occur due to the body’s increased energy expenditure as the tumor grows.
- Fatigue or Weakness:
– Tumors can lead to fatigue or weakness, especially if they interfere with the normal functioning of vital organs or cause the release of substances affecting the body’s metabolism.
Causes:
- Genetic Factors:
– Inherited genetic mutations can predispose individuals to the development of certain tumors. These genetic alterations can be passed down from one generation to the next.
- Environmental Factors:
– Exposure to environmental factors such as radiation, certain chemicals, or carcinogens can increase the risk of tumor development. This is common in cases of lung cancer due to tobacco smoke or skin cancer due to excessive sun exposure.
- Age:
– The risk of developing tumors often increases with age. Some tumors, such as certain types of cancer, are more prevalent in older individuals.
- Immune System Suppression:
– Conditions or medications that suppress the immune system can increase the risk of tumor development. A weakened immune system may not effectively control the growth of abnormal cells.
- Hormonal Factors:
– Hormonal imbalances or changes can contribute to the development of tumors, especially in tissues sensitive to hormonal fluctuations, such as the breast or uterus.
- Chronic Inflammation:
– Prolonged inflammation in a particular tissue or organ can create an environment conducive to tumor development. Chronic inflammatory conditions may increase the risk of certain cancers.
Types:
- Benign Tumor:
– Benign tumors are non-cancerous growths that do not invade nearby tissues or spread to other parts of the body. They typically have a well-defined boundary and are often localized.
- Malignant Tumor:
– Malignant tumors, commonly referred to as cancer, are characterized by uncontrolled growth and the potential to invade surrounding tissues or metastasize to other parts of the body. Malignant tumors can be life-threatening if not treated.
- Carcinoma:
– Carcinomas are malignant tumors that originate in epithelial tissues, which cover the body’s surfaces and line organs. Examples include lung carcinoma and breast carcinoma.
- Sarcoma:
– Sarcomas are malignant tumors that develop in connective tissues, including bones, muscles, and blood vessels. Osteosarcoma and leiomyosarcoma are examples of sarcomas.
- Lymphoma:
– Lymphomas are tumors that arise in the lymphatic system, including lymph nodes, spleen, and bone marrow. Hodgkin’s lymphoma and non-Hodgkin’s lymphoma are two main types.
- Leukemia:
– Leukemia is a type of cancer that affects the blood and bone marrow, leading to the uncontrolled production of abnormal blood cells. It is classified into acute and chronic forms.
- Central Nervous System Tumors:
– Tumors affecting the central nervous system (brain and spinal cord) can be either benign or malignant. Gliomas and meningiomas are common examples.
- Melanoma:
– Melanoma is a malignant tumor that develops in melanocytes, the pigment-producing cells in the skin. It is a type of skin cancer.
Ulcer
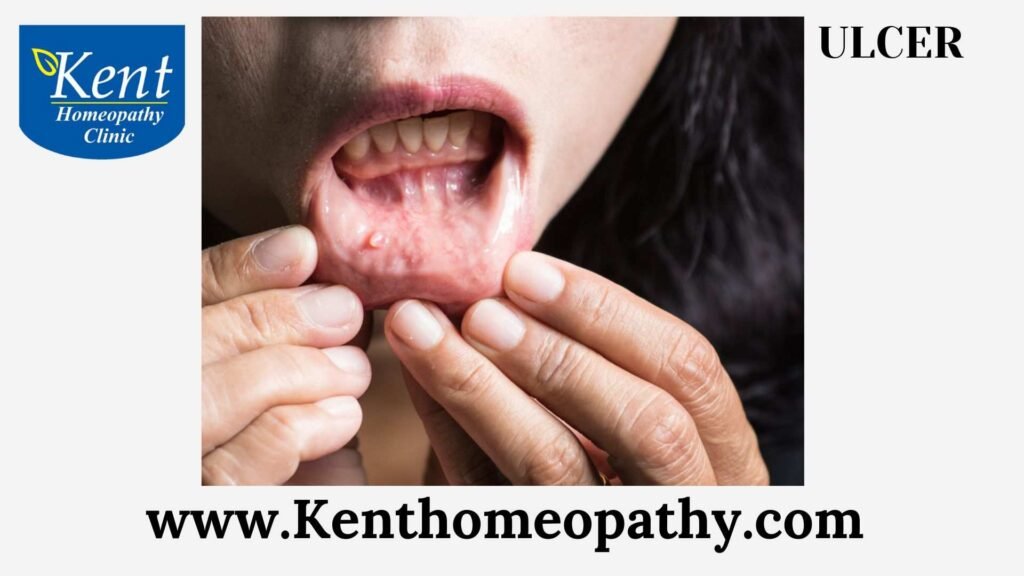
Ulcer
Ulcers: Unraveling Symptoms, Causes, and Types
An ulcer refers to a sore or lesion that forms on the skin or mucous membranes, commonly occurring in the gastrointestinal tract. Understanding the symptoms, causes, and types of ulcers is crucial for proper diagnosis and effective management.
Symptoms:
- Pain:
– Pain is a primary symptom of ulcers. The severity and nature of the pain can vary, ranging from a dull ache to sharp, burning pain. Pain is often felt in the affected area, such as the stomach or duodenum.
- Burning Sensation:
– A burning sensation is a characteristic symptom, especially in peptic ulcers affecting the stomach or upper part of the small intestine (duodenum).
- Indigestion:
– Ulcers can cause indigestion, leading to discomfort, bloating, and a feeling of fullness even after consuming a small amount of food.
- Nausea and Vomiting:
– Nausea and vomiting may occur, particularly in cases of gastric ulcers. Vomiting may sometimes contain blood or appear as “coffee grounds” if there is bleeding.
- Changes in Appetite:
– Ulcers can affect appetite, leading to changes in eating habits. Some individuals may experience a loss of appetite, while others may eat to alleviate the discomfort.
- Heartburn:
– Peptic ulcers in the esophagus can cause heartburn, a burning sensation in the chest. This symptom may be exacerbated by lying down or bending over.
- Weight Loss:
– Persistent ulcers can lead to weight loss, especially if the individual experiences a decreased appetite or avoids certain foods due to discomfort.
- Blood in Stool:
– Gastrointestinal ulcers, particularly those in the stomach or duodenum, may result in bleeding. This can lead to the presence of blood in the stool, which may appear dark or tarry.
Causes:
- Helicobacter pylori Infection:
– The bacterium Helicobacter pylori (H. pylori) is a common cause of peptic ulcers. It can weaken the protective lining of the stomach and duodenum, making them more susceptible to damage from stomach acids.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
– Regular use of NSAIDs, such as aspirin and ibuprofen, can irritate the stomach lining and increase the risk of developing ulcers. Long-term use of these medications is a significant risk factor.
- Smoking:
– Smoking has been associated with an increased risk of developing peptic ulcers and can delay the healing of existing ulcers.
- Excessive Alcohol Consumption:
– Excessive alcohol intake can irritate and erode the lining of the stomach and intestine, contributing to the development of ulcers.
- Stress:
– While stress does not directly cause ulcers, it can exacerbate existing conditions and delay the healing process. Stress management is essential for individuals prone to ulcers.
- Zollinger-Ellison Syndrome:
– Zollinger-Ellison syndrome is a rare condition characterized by tumors in the pancreas or duodenum, leading to excessive production of stomach acid. This can result in the development of multiple ulcers.
Types:
- Peptic Ulcers:
– Peptic ulcers are open sores that develop on the inner lining of the stomach (gastric ulcers) or the upper part of the small intestine (duodenal ulcers). These are the most common types of ulcers.
- Esophageal Ulcers:
– Esophageal ulcers occur in the lining of the esophagus, often as a result of gastroesophageal reflux disease (GERD). These ulcers can cause pain and difficulty swallowing.
- Stress Ulcers:
– Stress ulcers are associated with severe illness, trauma, or major surgery. These ulcers often develop in critically ill patients and can be challenging to manage.
- Curling Ulcers:
– Curling ulcers are a type of stress ulcer that specifically occurs in individuals with severe burns. They are believed to be linked to decreased blood flow to the stomach lining.
- Cushing Ulcers:
– Cushing ulcers are stress ulcers associated with head injuries or increased intracranial pressure. They can lead to rapid and severe bleeding.
- Venous Ulcers:
– Venous ulcers are typically found on the lower legs and are associated with poor circulation, often due to venous insufficiency. These ulcers can be chronic and challenging to heal.
Varicose veins

Varicose veins
Varicose Veins: Unraveling Symptoms, Causes, and Types
Varicose veins are enlarged, twisted veins that often appear blue or dark purple. They usually occur in the legs and are a common condition, affecting many people, especially as they age. Understanding the symptoms, causes, and types of varicose veins is essential for proper management and prevention of complications.
Symptoms:
- Visible, Bulging Veins:
– The primary visual symptom of varicose veins is the presence of swollen, bulging veins that are easily visible beneath the skin. They may appear twisted or rope-like.
- Discoloration of Skin:
– Over time, varicose veins can cause the skin around them to become discolored. This can result in a reddish or brownish appearance, indicating potential skin changes.
- Aching or Pain:
– Some individuals with varicose veins experience aching or pain in the affected area, especially after prolonged periods of standing or sitting. The pain may be described as throbbing or cramping.
- Heaviness or Fatigue:
– Many people with varicose veins report a sensation of heaviness or fatigue in the legs. This feeling is often more pronounced at the end of the day.
- Itching or Burning:
– Varicose veins can cause itching or a burning sensation in the skin overlying the affected veins. Scratching may lead to further complications.
- Swelling:
– Swelling, known as edema, can occur around the ankles and lower legs due to poor circulation associated with varicose veins.
- Restless Legs:
– Some individuals with varicose veins experience restless legs syndrome, characterized by an uncontrollable urge to move the legs, especially when at rest.
Causes:
- Faulty Valves in Veins:
– The primary cause of varicose veins is the malfunctioning of valves within the veins. Veins have one-way valves that help blood flow upward toward the heart. When these valves weaken or become damaged, blood can pool in the veins, leading to enlargement and twisting.
- Genetics:
– There is a strong genetic component to the development of varicose veins. If your parents or other family members have had varicose veins, you may be more prone to developing them.
- Age:
– Aging is a factor in the development of varicose veins. As people get older, the veins can lose elasticity, and the valves may become less efficient.
- Gender:
– Women are more likely to develop varicose veins than men. Hormonal changes associated with pregnancy, menstruation, and menopause can contribute to the development of varicose veins.
- Pregnancy:
– The increased volume of blood during pregnancy, combined with the pressure exerted by the growing uterus on pelvic veins, can contribute to the development of varicose veins.
- Obesity:
– Excess body weight places additional pressure on the veins, especially in the lower extremities, increasing the risk of varicose veins.
- Prolonged Standing or Sitting:
– Jobs or lifestyles that involve long periods of standing or sitting can impede blood circulation, contributing to the development of varicose veins.
Types:
- Primary Varicose Veins:
– Primary varicose veins refer to veins that develop independently without an underlying medical condition. They are often associated with genetic factors and aging.
- Secondary Varicose Veins:
– Secondary varicose veins are a result of an underlying condition, such as deep vein thrombosis (DVT) or pelvic vein obstruction. These conditions can affect the normal flow of blood in the veins.
- Trunk Varicose Veins:
– Trunk varicose veins involve the large veins near the surface of the skin, such as the great saphenous vein. These veins are often visible and may cause symptoms like pain and swelling.
- Reticular Varicose Veins:
– Reticular varicose veins are smaller, bluish veins located closer to the surface of the skin. They may appear as a network of veins and are often associated with cosmetic concerns.
- Telangiectasia (Spider Veins):
– Telangiectasia, commonly known as spider veins, are tiny, dilated blood vessels that appear close to the skin’s surface. They are often red or blue in color and can be a cosmetic concern.
- Pelvic Congestion Syndrome:
– Pelvic congestion syndrome involves varicose veins in the pelvic region. It can cause pelvic pain, especially in women, and may be associated with conditions like chronic pelvic pain and ovarian vein reflux.
Vertigo

Vertigo
Vertigo: Unraveling Symptoms, Causes, and Types
Vertigo is a sensation of spinning or dizziness, often described as feeling like the world is spinning around you. It is not a condition itself but a symptom of an underlying issue affecting the balance and spatial orientation systems in the inner ear or the brain. Understanding the symptoms, causes, and types of vertigo is essential for accurate diagnosis and appropriate management.
Symptoms:
- Spinning Sensation:
– The hallmark symptom of vertigo is a spinning sensation, as if the environment around you is rotating or moving.
- Nausea and Vomiting:
– Vertigo is commonly associated with nausea and vomiting, especially when the spinning sensation is severe.
- Sweating and Paleness:
– Individuals experiencing vertigo may exhibit signs of autonomic nervous system arousal, including sweating and paleness.
- Unsteady Gait:
– Vertigo can affect coordination and balance, leading to an unsteady gait. Individuals may stumble or have difficulty walking.
- Jerking Eye Movements (Nystagmus):
– Nystagmus, involuntary rapid eye movements, often accompanies vertigo. The eyes may move horizontally, vertically, or in a rotary fashion.
- Headache:
– Some people with vertigo may experience headaches, particularly if the condition is related to migraines or other primary headache disorders.
Causes:
- Inner Ear Disorders:
– Most cases of vertigo originate from disorders of the inner ear, including benign paroxysmal positional vertigo (BPPV), vestibular neuritis, and Meniere’s disease.
- BPPV (Benign Paroxysmal Positional Vertigo):
– BPPV occurs when tiny calcium crystals in the inner ear become dislodged and move into the semicircular canals, leading to vertigo triggered by specific head movements.
- Vestibular Neuritis:
– Vestibular neuritis is inflammation of the vestibular nerve, often caused by viral infections. It results in sudden-onset vertigo, along with nausea and imbalance.
- Meniere’s Disease:
– Meniere’s disease is characterized by fluid buildup in the inner ear, leading to episodes of vertigo, hearing loss, tinnitus (ringing in the ears), and a feeling of fullness in the ear.
- Migraines:
– Some individuals experience vertigo as part of a migraine episode, known as vestibular migraine. This can occur with or without a headache.
- Head or Neck Injuries:
– Trauma to the head or neck, such as a concussion or whiplash, can damage the vestibular system and lead to vertigo.
- Medications:
– Certain medications, especially those affecting the inner ear or central nervous system, can cause vertigo as a side effect.
- Infections:
– Infections affecting the inner ear, such as labyrinthitis, can result in vertigo. Viral or bacterial infections may be responsible.
- Central Nervous System Disorders:
– Conditions affecting the brain, such as tumors, strokes, or multiple sclerosis, can disrupt the normal functioning of the vestibular system, leading to vertigo.
Types:
- Peripheral Vertigo:
– Peripheral vertigo is associated with disorders of the inner ear or vestibular nerve. Common causes include BPPV, vestibular neuritis, and Meniere’s disease. Symptoms often include nystagmus and are usually triggered by specific head movements.
- Central Vertigo:
– Central vertigo is related to disorders in the central nervous system, particularly the brainstem or cerebellum. Causes may include migraines, brain tumors, or strokes. Central vertigo often presents with more sustained symptoms and may be associated with neurological signs beyond vertigo.
- Positional Vertigo:
– Positional vertigo, such as BPPV, is triggered by specific head movements or changes in position. The vertigo is often brief but intense and can be accompanied by nausea.
- Rotational Vertigo:
– Rotational vertigo refers to the sensation of spinning or rotation. Conditions like vestibular neuritis or Meniere’s disease can cause episodes of rotational vertigo.
- Non-Rotational Vertigo:
– Non-rotational vertigo may involve a feeling of swaying, tilting, or being pulled to one side without a clear sense of spinning. This type of vertigo is common in central nervous system disorders.
- Persistent Postural-Perceptual Dizziness (PPPD):
– PPPD is a chronic condition characterized by persistent dizziness or unsteadiness, often triggered by visual stimuli or changes in posture. It may follow an initial episode of vertigo.
Viral infection

Viral infection
Viral Infections: Unraveling Symptoms, Causes, and Types
Viral infections are illnesses caused by various types of viruses that invade and replicate within host cells. Viruses can affect different organs and systems in the body, leading to a wide range of symptoms. Understanding the symptoms, causes, and types of viral infections is crucial for effective prevention, diagnosis, and treatment.
Symptoms:
- Fever:
– Fever is a common symptom of viral infections. It indicates that the body is responding to the presence of the virus and is part of the immune system’s defense mechanism.
- Fatigue:
– Viral infections often cause fatigue and weakness, as the body redirects energy resources to fight the invading virus.
- Cough and Respiratory Symptoms:
– Many viral infections affect the respiratory system, leading to symptoms such as cough, sore throat, nasal congestion, and difficulty breathing.
- Body Aches and Muscle Pain:
– Body aches and muscle pain are frequent symptoms of viral infections, contributing to the overall feeling of discomfort.
- 5. Headache:
– Headaches are common with viral infections and can range from mild to severe, depending on the type and severity of the infection.
- Gastrointestinal Symptoms:
– Some viral infections, such as norovirus or rotavirus, can cause gastrointestinal symptoms like nausea, vomiting, diarrhea, and abdominal pain.
- Skin Rash:
– Certain viral infections, including measles or chickenpox, may present with a characteristic skin rash. The appearance of the rash varies based on the virus.
- Swollen Lymph Nodes:
– Viral infections often lead to the activation of the immune system, resulting in swollen lymph nodes, particularly in areas close to the infection site.
Causes:
- Viral Agents:
– Viral infections are caused by viruses, which are microscopic infectious agents. Viruses can be classified into various families, each with its own characteristics and ability to infect specific host cells.
- Transmission:
– Viral infections are typically transmitted from person to person through various means, including respiratory droplets, direct contact with infected individuals, contaminated surfaces, or through vectors like mosquitoes.
- Airborne Transmission:
– Some viruses, like influenza or the common cold viruses, can spread through airborne droplets when an infected person coughs or sneezes.
- Fecal-Oral Transmission:
– Certain viruses, such as norovirus or hepatitis A, can be transmitted through contaminated food, water, or surfaces that have come in contact with infected fecal matter.
- Vector-Borne Transmission:
– Mosquitoes, ticks, and other vectors can transmit viruses to humans. Examples include the Zika virus and dengue virus transmitted by mosquitoes.
- Vertical Transmission:
– Some viruses can be transmitted vertically from mother to child during pregnancy, childbirth, or breastfeeding. Examples include HIV and cytomegalovirus.
- Blood-Borne Transmission:
– Blood-borne viruses, like hepatitis B or C, can be transmitted through exposure to infected blood or blood products.
Types:
- Respiratory Viruses:
– Examples include influenza viruses, respiratory syncytial virus (RSV), rhinoviruses (cause of the common cold), and coronaviruses (including SARS-CoV-2 responsible for COVID-19).
- Gastrointestinal Viruses:
– Norovirus, rotavirus, and adenoviruses are examples of viruses that primarily affect the gastrointestinal system, leading to symptoms like vomiting and diarrhea.
- Herpesviruses:
– Herpesviruses include herpes simplex viruses (HSV-1 and HSV-2), varicella-zoster virus (causing chickenpox and shingles), and Epstein-Barr virus (associated with infectious mononucleosis).
- Flaviviruses:
– Flaviviruses include Zika virus, dengue virus, and West Nile virus. These are often transmitted by mosquitoes and can cause a range of symptoms from mild fever to severe neurological complications.
- Hepatitis Viruses:
– Hepatitis viruses, including hepatitis A, B, C, D, and E, primarily affect the liver and can lead to inflammation and damage.
- Human Immunodeficiency Virus (HIV):
– HIV attacks the immune system, specifically CD4 cells (T cells), and can lead to acquired immunodeficiency syndrome (AIDS) if left untreated.
- Poxviruses:
– Poxviruses include variola virus (smallpox) and vaccinia virus (used in smallpox vaccination). Smallpox has been eradicated, but other poxviruses can cause infections in animals and humans.
- Arboviruses:
– Arboviruses, transmitted by arthropods like mosquitoes and ticks, include viruses such as West Nile virus, Zika virus, and chikungunya virus.
Contact to know more
Contact
Timings
Monday to Saturday:
11:00 AM to 02:30 PM
06:30 PM to 09:00 PM
