Abscess

Abscess
An abscess is a localized collection of pus, typically caused by a bacterial infection. It forms when the body’s immune system attempts to isolate and eliminate invading microorganisms. The pus, consisting of dead white blood cells, tissue debris, and bacteria, accumulates in a confined space, leading to swelling, pain, and sometimes redness. Abscesses can occur in various body parts, such as skin, internal organs, or teeth.
Causes of Abscess:
- Bacterial Infections:
– Most common cause, with Staphylococcus aureus being a frequent culprit.
– Bacteria infiltrate through wounds, cuts, or compromised tissues, triggering an immune response.
- Weakened Immune System:
– Conditions like diabetes, HIV, or immune-suppressing medications increase susceptibility to infections.
– Impaired immune response allows bacteria to proliferate, contributing to abscess formation.
- Poor Hygiene:
– Inadequate cleanliness creates an environment conducive to bacterial growth.
– Lack of proper hygiene can lead to skin infections, contributing to abscess development.
- Obstructed Glands or Hair Follicles:
– Blockages in sweat glands or hair follicles prevent normal drainage.
– Accumulation of secretions and bacteria promotes abscess formation.
Symptoms of Abscess:
- Localized Pain:
– Throbbing or aching pain at the site of infection.
– Pain intensity may increase as the abscess enlarges.
- Swelling:
– Visible swelling due to the accumulation of pus and inflammatory response.
– Swelling can cause discomfort and restrict movement in the affected area.
- Redness and Heat:
– Inflammation leads to increased blood flow, causing redness.
– The affected area feels warm due to the inflammatory process.
- Tenderness:
– Increased sensitivity and discomfort upon touch.
– Tenderness is a common symptom, especially as the abscess expands.
- Fever:
– Systemic response to infection, causing an elevated body temperature.
– Fever may accompany more severe or deep-seated abscesses.
- Chills and Malaise:
– Systemic symptoms indicating the body’s response to infection.
– Chills, fatigue, and a general feeling of illness may be present.
Types of Abscess:
- Skin Abscess:
– Develops beneath the skin surface.
– Often occurs in hair follicles or sweat glands.
– Presents as a painful, swollen lump filled with pus.
- Dental Abscess:
– Occurs within teeth or gums, usually due to untreated cavities or dental infections.
– Causes severe toothache, swelling, and often results in pus drainage.
- Peritonsillar Abscess:
– Forms near the tonsils, often as a complication of tonsillitis.
– Symptoms include severe throat pain, difficulty swallowing, and swollen neck glands.
- Brain Abscess:
– Uncommon but serious, typically resulting from infections spreading from other parts of the body.
– Presents with headaches, neurological symptoms, and fever.
- Liver Abscess:
– Usually caused by bacterial infection, often originating from the digestive tract.
– Symptoms include abdominal pain, fever, and jaundice.
- Spinal Abscess:
– Develops around the spinal cord, often due to bacterial infection.
– Presents with back pain, neurological deficits, and fever.
- Breast Abscess:
– Commonly associated with breastfeeding complications such as mastitis.
– Causes breast pain, redness, and localized swelling.
– Complications:
– Without prompt treatment, abscesses can lead to the spread of infection to surrounding tissues or bloodstream.
– Systemic complications include sepsis, a potentially life-threatening condition.
– Recurrent abscesses may indicate underlying health issues that require further investigation.
Early detection and proper management are crucial to prevent complications and promote a successful recovery. Seeking medical attention when symptoms arise is essential for effective treatment and minimizing the impact of abscess-related complications.
Acne

Acne
Acne is a common skin condition characterized by the formation of pimples, blackheads, whiteheads, cysts, and nodules. It primarily affects the face, chest, back, and shoulders. While it is most prevalent among teenagers, acne can persist into adulthood and may vary in severity.
Symptoms:
The symptoms of acne encompass a range of skin blemishes, including:
- Pimples: Small red bumps that may contain pus.
- Blackheads: Open pores with darkened masses of skin debris.
- Whiteheads: Closed pores with small, flesh-colored bumps.
- Cysts and nodules: Deeper, painful lumps beneath the skin’s surface.
Causes:
Several factors contribute to the development of acne:
- Excess oil production: Overactive oil glands can clog hair follicles, leading to acne.
- Clogged pores: Dead skin cells and excess oil can block hair follicles, creating an environment for acne-causing bacteria to thrive.
- Bacteria: Propionibacterium acnes, a bacteria that normally lives on the skin, can multiply in clogged hair follicles and trigger inflammation.
- Hormonal changes: Fluctuations in hormones, particularly during puberty, menstruation, pregnancy, and the use of certain contraceptives, can contribute to acne.
- Genetics: A family history of acne may increase the likelihood of developing the condition.
- Diet: While the link is not fully understood, some studies suggest that certain diets high in sugar and dairy may exacerbate acne for some individuals.
- Stress: While not a direct cause, stress can aggravate existing acne.
Types of Acne:
- Acne Vulgaris: The most common type, characterized by blackheads, whiteheads, pimples, and sometimes cysts.
- Comedonal Acne: Primarily blackheads and whiteheads without much inflammation.
- Inflammatory Acne: Characterized by red and swollen pimples, often with pus.
- Nodular Acne: Large, painful nodules beneath the skin’s surface.
- Cystic Acne: Severe, deep-seated cysts, the most serious form of acne.
Prevention:
While not entirely preventable, certain measures can help manage and reduce the risk of acne:
- Regular Cleansing: Gently cleanse the skin to remove excess oil and debris.
- Avoiding Picking or Squeezing: This can worsen inflammation and lead to scarring.
- Choosing Cosmetics Carefully: Non-comedogenic products are less likely to clog pores.
- Managing Stress: Stress reduction techniques can contribute to overall skin health.
In conclusion, acne is a multifactorial skin condition influenced by genetic, hormonal, and environmental factors. Understanding the symptoms, causes, and types of acne is crucial for effective management and prevention. Seeking professional advice is recommended for tailored treatment plans based on individual needs and severity.
Alopecia Areata (Alopecia)

Alopecia Areata (Alopecia)
Alopecia Areata: Unveiling Symptoms, Causes, and Types
Alopecia areata is a common autoimmune disorder that leads to hair loss on the scalp and other areas of the body. This condition occurs when the immune system mistakenly attacks hair follicles, causing them to shrink and slow down hair production. The extent and pattern of hair loss can vary, ranging from small, round patches to extensive baldness.
Symptoms:
- Hair Loss: The primary symptom is sudden hair loss, often in small, round patches. Hair loss can occur on the scalp, face, and other parts of the body.
- Smooth, Bald Patches: Affected areas typically show smooth skin without visible hair follicles.
- Nail Changes: In some cases, changes in the nails, such as pitting or ridges, may accompany alopecia areata.
Causes:
- Autoimmune Reaction: Alopecia areata is considered an autoimmune disorder where the immune system mistakenly targets the body’s own cells, in this case, the hair follicles.
- Genetic Predisposition: There is evidence that a genetic component may play a role, as individuals with a family history of autoimmune diseases or alopecia areata have an increased risk.
- Environmental Triggers: Environmental factors, such as viral infections or severe stress, may act as triggers for the onset of alopecia areata in genetically predisposed individuals.
- Immune System Dysfunction: The exact mechanism by which the immune system attacks hair follicles is not fully understood, but it leads to inflammation and hair loss.
Types of Alopecia Areata:
- Alopecia Areata (Patchy): This is the most common form, characterized by round patches of hair loss on the scalp or other parts of the body. Hair loss may be limited, or it can progress to more extensive areas.
- Alopecia Totalis: In this type, hair loss involves the entire scalp, leading to complete baldness on the head.
- Alopecia Universalis: The most severe form, alopecia universalis results in total body hair loss, including the scalp, face, and body.
- Ophiasis Pattern: Hair loss occurs in a wave-like pattern along the edges of the scalp, resembling a band. This pattern is more challenging to treat.
Prognosis:
– Alopecia areata is unpredictable, and the course of the condition can vary widely. Spontaneous regrowth of hair is possible, even after extensive hair loss.
– In some cases, hair may regrow but then fall out again. The likelihood of recurrence and the extent of regrowth are highly individual.
In summary, alopecia areata is an autoimmune condition that results in hair loss, impacting individuals physically and emotionally. Understanding the symptoms, causes, types, and available treatments is crucial for managing the condition and providing support to those affected.
Acne Rosacea

Acne Rosacea
Acne rosacea, commonly referred to as rosacea, is a chronic skin condition that primarily affects the face. It is characterized by redness, visible blood vessels, and the development of pimple-like bumps. Unlike traditional acne, rosacea tends to occur in adults and has distinctive features. Understanding its symptoms, causes, and types is essential for proper diagnosis and management.
Symptoms:
- Facial Redness: Persistent redness, often resembling a sunburn, is a hallmark symptom.
- Flushing: Episodes of facial redness that come and go, often triggered by factors like spicy foods, alcohol, or sun exposure.
- Pimple-like Bumps: Small, red bumps resembling acne papules and pustules may develop, especially in the central face.
- Visible Blood Vessels: Small blood vessels (telangiectasia) become visible on the skin.
- Eye Irritation: In some cases, rosacea can affect the eyes, causing dryness, irritation, and a gritty sensation.
- Enlarged Nose: In severe cases, rhinophyma may occur, causing thickening and enlargement of the nose tissue.
Causes:
The exact cause of rosacea is not fully understood, but several factors contribute to its development:
- Vascular Dysfunction: Abnormalities in blood vessels, leading to increased blood flow and facial redness.
- Genetics: Family history may play a role in predisposing individuals to rosacea.
- Dermatitis Mites: The presence of microscopic mites (Demodex folliculorum) on the skin may be associated with rosacea, though their exact role is still under investigation.
- Abnormal Immune Response: Inflammation triggered by an overactive immune system may contribute to the symptoms.
- Triggers: Certain environmental and lifestyle factors, such as sun exposure, spicy foods, alcohol, stress, and hot beverages, can exacerbate rosacea.
Types of Acne Rosacea:
- Erythematotelangiectatic Rosacea: Characterized by persistent facial redness, visible blood vessels, and occasional flushing.
- Papulopustular Rosacea: In addition to redness and blood vessels, this type involves pimple-like bumps and pus-filled lesions, resembling acne.
- Phymatous Rosacea: This rare subtype leads to thickening and enlargement of facial tissues, particularly the nose (rhinophyma).
- Ocular Rosacea:Affecting the eyes, symptoms include dryness, irritation, and redness.
Anhidrosis

Anhidrosis
Anhidrosis is a medical condition characterized by the inability to sweat properly. Sweating is a vital mechanism that helps regulate body temperature by dissipating heat through the evaporation of sweat from the skin’s surface. When anhidrosis occurs, the body loses its ability to cool down efficiently, which can lead to potentially serious consequences, such as overheating.
Symptoms:
The primary symptom of anhidrosis is the reduced or absence of sweating. Individuals with anhidrosis may experience dry skin, elevated body temperature, and a lack of moisture on the skin’s surface. Since sweating is essential for cooling the body during physical exertion or exposure to heat, affected individuals may be prone to heat-related illnesses, such as heat exhaustion or heatstroke. Additionally, they may have difficulty tolerating hot environments and may exhibit flushed skin.
Causes:
There are several potential causes of anhidrosis, and they can be broadly categorized into neurological, dermatological, and systemic factors.
- Neurological Causes:
– Peripheral Neuropathy: Damage to the nerves that control sweating can result in anhidrosis. Conditions such as diabetes, autoimmune disorders, or traumatic injuries can contribute to peripheral neuropathy.
– Autonomic Nervous System Dysfunction: The autonomic nervous system regulates involuntary bodily functions, including sweating. Dysfunction in this system due to conditions like multiple system atrophy or Parkinson’s disease can lead to anhidrosis.
- Dermatological Causes:
– Skin Damage or Diseases: Skin conditions such as burns, infections, or certain dermatological disorders can impair the sweat glands, preventing normal sweating.
– Scarring: Scarring from injuries or surgeries may interfere with the function of sweat glands.
- Systemic Causes:
– Dehydration: Inadequate fluid intake can reduce the body’s ability to produce sweat.
– Medications: Certain medications, such as anticholinergic drugs or beta-blockers, may interfere with the sweating process as a side effect.
– Genetic Factors: In rare cases, genetic factors may contribute to anhidrosis.
Types:
Anhidrosis can be classified based on its extent and distribution across the body.
- Localized Anhidrosis: This type involves the loss of sweating in specific areas of the body. It may be caused by localized nerve damage or skin conditions affecting specific regions.
- Generalized Anhidrosis: Generalized anhidrosis affects larger areas or the entire body. It is often associated with systemic conditions, such as certain neurological disorders or dehydration.
- Hypohidrosis: This refers to reduced sweating rather than complete absence. Individuals with hypohidrosis may still produce some sweat, but the amount is significantly lower than normal.
In diagnosing anhidrosis, healthcare professionals may conduct a thorough medical history review, physical examination, and, if necessary, specialized tests such as thermoregulatory sweat testing. Treatment depends on the underlying cause, and addressing the root issue is crucial. For example, managing diabetes, treating skin conditions, or adjusting medications may help alleviate anhidrosis symptoms.
In summary, anhidrosis is a condition characterized by the inability to sweat properly, posing challenges to the body’s natural cooling mechanism. Understanding its symptoms, causes, and types is essential for accurate diagnosis and targeted treatment to address the underlying factors contributing to this condition.
Athlete's Foot

Athlete's Foot
Athlete’s Foot: Unveiling the Fungal Menace
Athlete’s foot, medically known as tinea pedis, is a common fungal infection affecting the skin of the feet. This condition, prevalent among athletes and others who frequently use communal showers or pools, is caused by various fungi, particularly those belonging to the dermatophyte group. Understanding the symptoms, types, and causes of athlete’s foot is essential for effective management and prevention.
Symptoms of Athlete’s Foot:
- Itching: Persistent itching, often severe, is a primary symptom of athlete’s foot. It can occur between the toes or on the soles of the feet.
- Redness and Inflammation: The infected skin may appear red, swollen, and inflamed, contributing to discomfort.
- Cracking and Peeling: The skin affected by athlete’s foot may crack or peel, leading to the formation of small, painful fissures.
- Blisters: Fluid-filled blisters, resembling small bubbles, can develop and contribute to further irritation.
- Burning Sensation: Some individuals may experience a burning or stinging sensation on the affected areas.
- Odor: Fungal infections can produce an unpleasant odor, particularly when the feet are enclosed in shoes for an extended period.
These symptoms can vary in intensity, and the infection may affect one or both feet. In severe cases, the fungus can spread to the toenails, leading to additional complications.
Types of Athlete’s Foot:
- Interdigital Athlete’s Foot (Toe Web Infection):
– This is the most common type, affecting the skin between the toes.
– It often presents as redness, itching, and the formation of small, fluid-filled blisters.
- Moccasin-Type Athlete’s Foot:
– This form of infection typically begins with a dry, scaly rash on the soles of the feet, resembling a moccasin.
– It can gradually extend to the sides of the feet and may involve the toenails.
- Vesicular Athlete’s Foot:
– Characterized by the development of fluid-filled blisters on the soles of the feet.
– The blisters may be itchy and can contribute to the spread of the infection.
- Ulcerative Athlete’s Foot:
– In rare cases, athlete’s foot can lead to the formation of ulcers on the affected skin.
– Ulcerative athlete’s foot may cause pain and increase the risk of secondary bacterial infections.
Causes of Athlete’s Foot:
- Fungal Infections:
– Athlete’s foot is primarily caused by fungi, including Trichophyton, Epidermophyton, and Microsporum species.
– These fungi thrive in warm, moist environments, such as locker rooms, showers, and swimming pools.
- Direct Contact:
– The fungus responsible for athlete’s foot is often spread through direct contact with infected skin or by sharing contaminated items like towels, socks, or shoes.
- Warm and Moist Environments:
– Fungi responsible for athlete’s foot thrive in warm and moist conditions.
– Wearing damp socks or shoes and not allowing feet to dry properly can contribute to fungal growth.
- Weakened Immune System:
– Individuals with weakened immune systems, whether due to certain medical conditions or medications, may be more susceptible to fungal infections, including athlete’s foot.
- Poor Hygiene:
– Inadequate foot hygiene, such as not washing and drying feet properly, can increase the risk of fungal infections.
- Footwear:
– Wearing tight, closed shoes for prolonged periods can create an environment conducive to fungal growth.
– Shoes that do not allow proper ventilation contribute to the persistence of athlete’s foot.
Conclusion:
Athlete’s foot, though common, can be effectively managed and prevented with proper hygiene practices and prompt treatment. Recognizing the symptoms, understanding the types, and addressing the underlying causes are crucial steps in ensuring relief from this fungal menace. If symptoms persist or worsen, consulting a healthcare professional for appropriate diagnosis and treatment is recommended.
Atopic Dermatitis

Atopic Dermatitis
Atopic dermatitis, commonly known as eczema, is a chronic inflammatory skin condition that manifests as dry, itchy skin with red rashes. It often occurs in individuals with a predisposition to allergic conditions and can vary in severity from mild to severe. Understanding the symptoms, causes, and types of atopic dermatitis is crucial for effective management and treatment.
Symptoms:
The symptoms of atopic dermatitis can vary widely among individuals, but common manifestations include:
- Itchy Skin: Persistent itching is a hallmark symptom of atopic dermatitis, and scratching can exacerbate the condition.
- Dry and Red Skin: Affected areas often appear dry and red, with inflammation contributing to the characteristic appearance of eczematous skin.
- Rashes: Eczema rashes can take different forms, including patches of red or brownish-gray skin, raised bumps, or small, fluid-filled blisters that may ooze and crust over.
- Swelling: In some cases, the skin may become swollen, particularly around the affected areas.
- Cracking and Scaling: The skin may crack, especially in areas with repeated scratching, and show signs of scaling.
- Thickened Skin: With chronic or severe cases, the skin may become thickened and leathery, a condition known as lichenification.
Causes:
While the exact cause of atopic dermatitis is not fully understood, a combination of genetic, environmental, and immune system factors is believed to contribute to its development. Key factors include:
- Genetic Predisposition: Individuals with a family history of atopic conditions, such as asthma, hay fever, or other types of eczema, may have a higher risk of developing atopic dermatitis. Specific genetic variations are associated with an increased susceptibility to the condition.
- Immune System Dysfunction: Atopic dermatitis is linked to an abnormal immune response, where the immune system reacts excessively to triggers that are usually harmless. This heightened immune response contributes to inflammation and skin damage.
- Environmental Factors: Environmental factors can trigger or worsen atopic dermatitis symptoms. These include exposure to irritants like harsh soaps, detergents, or certain fabrics, as well as allergens like dust mites, pet dander, and pollen.
- Dysfunctional Skin Barrier: Individuals with atopic dermatitis often have a compromised skin barrier, making their skin more susceptible to irritants and allergens. This can result in increased water loss from the skin, leading to dryness and susceptibility to infections.
Types:
Atopic dermatitis can be categorized into different types based on the age of onset and the distribution of symptoms:
- Infantile Eczema: This type typically begins during infancy, often appearing between 2 and 6 months of age. It commonly affects the face, scalp, and extensor surfaces of the arms and legs.
- Childhood Eczema: As children grow, eczema may persist, change in appearance, or affect different areas of the body. The flexural areas, such as the creases of elbows and knees, are commonly affected.
- Adult-Onset Eczema: In some cases, atopic dermatitis can first appear in adulthood. It often presents as chronic, itchy skin in the flexural areas, as well as on the hands and feet.
- Localized Eczema: While atopic dermatitis often involves widespread areas of the body, it can also manifest in localized forms, affecting specific regions like the hands (hand eczema) or the face.
Management of atopic dermatitis involves a combination of preventive measures, such as avoiding triggers and maintaining good skincare practices, and medical interventions, including topical corticosteroids, moisturizers, and, in severe cases, systemic medications. While atopic dermatitis is a chronic condition, effective management strategies can help control symptoms and improve the quality of life for those affected. Seeking guidance from healthcare professionals is essential for a personalized and comprehensive approach to treatment.
Bacterial Skin Infection

Bacterial Skin Infection
Bacterial skin infections are conditions in which bacteria invade the skin, leading to various symptoms and manifestations. These infections can range from mild to severe and may affect different layers of the skin. Understanding the symptoms, causes, and types of bacterial skin infections is crucial for accurate diagnosis and effective treatment.
Symptoms:
The symptoms of bacterial skin infections can vary depending on the type of bacteria involved, the location of the infection, and the individual’s overall health. Common symptoms include:
- Redness and Swelling: Bacterial infections often cause redness and swelling in the affected area. The skin may appear inflamed and warm to the touch.
- Pain or Tenderness: Pain or tenderness may be present, especially if the infection involves deeper layers of the skin or underlying tissues.
- Pus or Drainage: Many bacterial skin infections result in the formation of pus or other types of drainage. Pus is a sign of the body’s immune response to the infection.
- Itching or Irritation: Itching is a common symptom, and the affected area may feel irritated or uncomfortable.
- 5. Fever: Systemic symptoms like fever may occur in more severe cases, indicating that the infection has spread beyond the skin.
- Skin Lesions or Rash: Depending on the specific bacteria causing the infection, various skin lesions or rashes may develop. These can include pustules, boils, impetigo, cellulitis, or abscesses.
Causes:
Bacterial skin infections are caused by the invasion of bacteria into the skin’s tissues. The most common culprits are Staphylococcus aureus and Streptococcus pyogenes, but other bacteria can also be responsible. The causes include:
- Breaks in the Skin: Bacteria can enter the skin through cuts, wounds, or other breaks in the skin’s protective barrier. This can happen through injuries, surgical incisions, or skin conditions like eczema.
- Skin Conditions: Certain skin conditions, such as dermatitis or psoriasis, can compromise the integrity of the skin, making it more susceptible to bacterial invasion.
- Poor Hygiene: Lack of proper hygiene practices can contribute to the growth and spread of bacteria on the skin, increasing the risk of infections.
- Close Contact: Bacterial skin infections can be spread through close person-to-person contact or by sharing contaminated items like towels, razors, or personal care products.
- Immune System Weakening: Conditions that weaken the immune system, such as diabetes, HIV/AIDS, or immunosuppressive medications, can increase susceptibility to bacterial skin infections.
Types:
Several types of bacterial skin infections are characterized by distinct symptoms and features:
- Impetigo: This highly contagious infection is commonly seen in children. It presents as red sores or blisters that may ooze and form a characteristic honey-colored crust.
- Cellulitis: Cellulitis is a bacterial infection affecting the deeper layers of the skin. It often causes redness, swelling, and tenderness. If left untreated, cellulitis can spread and lead to more severe complications.
- Folliculitis: Folliculitis occurs when hair follicles become inflamed due to bacterial infection. It can result in red, itchy bumps or pustules around hair follicles.
- Boils and Carbuncles: Boils are painful, pus-filled lumps that form beneath the skin. When multiple boils merge, they form a larger, deeper infection known as a carbuncle.
- Abscesses: An abscess is a collection of pus that forms within tissues. It can be caused by bacterial infection and often requires drainage for resolution.
- Erysipelas: This infection is characterized by a well-defined, raised rash with a clear border. It usually affects the face or lower legs and is caused by Streptococcus bacteria.
- Staphylococcal Scalded Skin Syndrome (SSSS): SSSS is a serious condition caused by certain strains of Staphylococcus aureus. It leads to widespread redness, peeling, and a scalded appearance of the skin.
- Necrotizing Fasciitis: This is a rare but severe bacterial infection that can rapidly destroy skin, subcutaneous tissues, and fascia. It requires immediate medical attention.
Treatment for bacterial skin infections typically involves antibiotics, either topical or oral, depending on the severity and type of infection. Proper wound care, hygiene practices, and avoiding contact with potentially contaminated surfaces can help prevent bacterial skin infections. In severe cases or when systemic symptoms are present, medical attention should be sought promptly for a thorough evaluation and appropriate management.
Barber's Itch

Barber's Itch
Barber’s itch, also known as Tinea barbae, is a fungal infection of the hair follicles in the beard and mustache area. It is caused by various dermatophyte fungi, primarily Trichophyton and Microsporum species. This condition is distinct from a bacterial infection and is characterized by its fungal origin. Understanding the symptoms, causes, and types of barber’s itch is essential for proper diagnosis and effective treatment.
Symptoms:
The symptoms of barber’s itch can vary in intensity, and affected individuals may experience the following:
- Red, Pimple-Like Bumps: Barber’s itch often begins with the appearance of small, red, and pimple-like bumps around the hair follicles in the beard and mustache area. These bumps may be itchy and may progress in severity.
- Pustules and Pus-filled Lesions: As the infection advances, pustules or small pockets of pus may develop. These can be tender and may rupture, releasing the pus.
- Itching and Discomfort: Itching is a common symptom of barber’s itch. The affected area may also be uncomfortable or sore, especially when touched.
- Swelling and Inflammation: The skin in the affected region may become swollen and inflamed, contributing to the discomfort associated with the condition.
- Crust Formation: In more severe cases, crusts or scales may form around the affected hair follicles. These crusts can contribute to the appearance of the infected area.
It’s important to note that barber’s itch is contagious and can spread through direct contact with infected individuals or contaminated items such as towels, combs, or razors.
Causes:
Barber’s itch is caused by dermatophyte fungi, which thrive in warm, humid environments. The primary causative agents are Trichophyton verrucosum, Trichophyton mentagrophytes, and Microsporum canis. The following factors contribute to the development of barber’s itch:
- Fungal Infection: The infection occurs when dermatophyte fungi penetrate the hair follicles in the beard and mustache area. These fungi thrive in warm, moist conditions and are often transmitted through direct contact with infected individuals or contaminated items.
- Poor Hygiene Practices: Inadequate hygiene, such as infrequent washing of the beard and mustache, can create an environment conducive to fungal growth.
- Close Shaving: Shaving too closely or using shared razors that may carry fungal spores can contribute to the development and spread of barber’s itch.
- Contact with Infected Animals: In some cases, contact with infected animals, particularly livestock, can lead to the transmission of dermatophyte fungi responsible for barber’s itch.
Types:
Barber’s itch can be categorized based on its clinical presentation and the specific fungi involved:
- Superficial Folliculitis: This is the milder form of barber’s itch, primarily involving the upper part of the hair follicle. It presents with pustules, redness, and itching.
- Deep Folliculitis: In more severe cases, the infection can extend deeper into the hair follicles, leading to deeper inflammation and larger, more tender pustules.
- Kerion: Kerion is an inflammatory and pustular form of barber’s itch that may result in painful, boggy swellings with crusting and drainage. It represents a more severe manifestation of the infection.
- Tinea Barbae Corporis: This type involves a more widespread fungal infection of the skin beyond the beard area. It may extend to the neck, chest, and other adjacent regions.
If symptoms persist or worsen despite initial treatment efforts, it is advisable to seek medical attention for a comprehensive evaluation and adjustment of the treatment plan. It’s also essential to inform close contacts, such as family members or individuals sharing living spaces, to prevent further spread of the infection. Taking preventive measures, practicing good personal hygiene, and avoiding direct contact with infected individuals or items can help reduce the risk of barber’s itch.
Bedbug Bites

Bedbug Bites
Bedbug bites are skin reactions resulting from the bites of bedbugs (Cimex lectularius). These small, reddish-brown insects feed on the blood of humans and animals during the night. While bedbugs are not known to transmit diseases, their bites can cause discomfort and skin reactions in some individuals. Understanding the symptoms, causes, and types of bedbug bites can help in identifying and managing these bites.
Symptoms:
The symptoms of bedbug bites can vary from person to person, and not everyone reacts to bedbug bites in the same way. Common symptoms include:
- Red, Itchy Bumps: Bedbug bites typically appear as small, red bumps on the skin. They are often itchy and can be grouped together in a line or cluster.
- Swelling: The affected area may become swollen due to the body’s inflammatory response to the bites.
- Red or Dark Spots: Some individuals may develop red or dark spots in the center of the bite marks. These spots can result from the bedbug’s feeding process.
- Itching: Bedbug bites are known for causing itching, which can range from mild to intense. Excessive scratching can lead to secondary infections.
- Linear or Clustered Pattern: Bedbug bites often appear in a linear or clustered pattern, as bedbugs tend to bite multiple times in close proximity.
It’s important to note that while bedbug bites share some similarities with other insect bites, they do not have a distinctive appearance, making it challenging to diagnose based solely on the appearance of the bites.
Causes:
The primary cause of bedbug bites is the feeding behavior of bedbugs. Bedbugs are nocturnal insects that feed on blood by piercing the skin with their mouthparts and withdrawing blood for several minutes. The causes of bedbug bites include:
- Bedbug Feeding: Bedbugs are attracted to the warmth and carbon dioxide emitted by humans, making them more active during the night. They typically bite exposed areas of skin while individuals are asleep.
- Infestation: Bedbug bites occur when there is a bedbug infestation in the sleeping or resting area. Bedbugs hide in cracks, crevices, and furniture during the day and come out at night to feed.
- Travel or Infested Environment: Individuals may experience bedbug bites after staying in infested accommodations, using infested furniture, or residing in an environment with a bedbug infestation.
- Clothing or Luggage Infestation: Bedbugs can also infest clothing, bedding, and luggage, allowing them to be transported to new locations. Bites may occur when the infested items are used or unpacked.
- Lack of Awareness: Bedbug bites may go unnoticed initially, and individuals may not realize they are being bitten until an infestation has progressed.
Types:
While bedbug bites themselves do not have distinct types, the reactions and severity of symptoms can vary among individuals. Some people may not react at all to bedbug bites, while others may experience more pronounced symptoms. Types of reactions to bedbug bites include:
- 1. Mild Reactions: Some individuals may have mild or no reactions to bedbug bites. They may not experience significant itching or swelling, making it difficult to detect the presence of bedbugs.
- Localized Reactions: Many people experience localized reactions, characterized by red, itchy bumps in the bitten area. The itching may be bothersome but usually resolves without severe complications.
- Allergic Reactions: In rare cases, individuals may be allergic to components in bedbug saliva, leading to more severe allergic reactions. These reactions may include widespread hives, difficulty breathing, or anaphylaxis, requiring immediate medical attention.
- Secondary Infections: Excessive scratching of bedbug bites can break the skin, increasing the risk of secondary bacterial infections. Infected bites may become red, swollen, and painful, requiring medical treatment.
It’s important to distinguish between bedbug bites and bites from other insects or skin conditions. Bedbug bites are not known to transmit diseases, but their presence can cause psychological distress and disrupt sleep. If an individual suspects bedbug bites or encounters signs of a bedbug infestation, it is advisable to seek professional pest control services for thorough inspection and treatment.
Managing bedbug bites involves avoiding excessive scratching to prevent secondary infections. Over-the-counter creams or antihistamines can help alleviate itching and inflammation. In cases of severe allergic reactions or secondary infections, medical consultation is recommended.
Preventing bedbug bites involves taking measures to avoid infestations, such as regularly inspecting and cleaning sleeping areas, using protective covers on mattresses and pillows, and being cautious when staying in unfamiliar accommodations. If there is concern about bedbug bites or an infestation, consulting with a healthcare professional or a pest control specialist is recommended for appropriate guidance and intervention.
Boils

Boils
Boils, also known as furuncles, are painful and often inflamed lumps that form on the skin. These skin infections arise from bacterial invasion of hair follicles or oil glands. Boils can be discomforting and may vary in size and severity, occurring either as isolated lesions or in clusters. Understanding the symptoms, causes, and types of boils is crucial for effective management and prevention.
Symptoms:
Boils typically present with distinctive symptoms that evolve as the infection progresses. Common symptoms include:
- Pain and Tenderness: Boils are characterized by localized pain and tenderness at the site of the infection. As the boil enlarges, the pain may intensify.
- Red, Swollen Bump: A noticeable red, swollen, and raised bump is a hallmark of a boil. The surrounding skin may also appear reddish.
- Pus Formation: Boils contain pus, which is a collection of dead white blood cells, bacteria, and tissue debris. The presence of pus gives the boil a yellow or whitish appearance at its center.
- Development of a Head: As a boil matures, it may develop a visible white or yellow head at the center. This indicates that the boil is ready to drain.
- Fever: In more severe cases, individuals with large boils may experience a low-grade fever.
- Spreading and Clustering: Boils can occur individually or cluster in specific areas such as the armpits, groin, buttocks, face, or neck. When boils cluster, they are known as carbuncles.
Causes:
The primary cause of boils is a bacterial infection, most commonly attributed to Staphylococcus aureus. Several factors contribute to the development of boils:
- Bacterial Infection: The entry of bacteria into hair follicles or oil glands, particularly Staphylococcus aureus, leads to infection and the formation of boils.
- Damaged Hair Follicles: Cuts, nicks, or other forms of damage to hair follicles create entry points for bacteria, increasing the likelihood of infection.
- Poor Hygiene: Inadequate personal hygiene can contribute to the accumulation of bacteria on the skin, raising the risk of boils.
- Close Contact: Skin-to-skin contact with an individual who has a boil or carries Staphylococcus aureus increases the risk of transmission.
- Compromised Immune System: Weakened immune systems, as seen in conditions like diabetes, HIV, or due to immunosuppressive medications, elevate susceptibility to bacterial infections, including boils.
- Friction or Irritation: Friction from tight clothing or repeated rubbing of the skin can irritate hair follicles, increasing the likelihood of boils.
- Poor Nutrition: Inadequate nutrition, especially deficiencies in vitamins and minerals, can compromise the immune system, heightening vulnerability to skin infections.
- Chronic Skin Conditions: Conditions like eczema or acne can compromise the skin barrier, making it easier for bacteria to enter and cause infection.
Types:
Boils come in different types, each with distinct characteristics:
- Furuncle: A furuncle is a single boil that develops around a hair follicle. It typically starts as a painful lump that enlarges, fills with pus, and eventually forms a visible head.
- Carbuncle: A carbuncle is a cluster of furuncles, often situated deeper in the skin. Carbuncles are larger and may cause more severe symptoms than individual furuncles.
- Pilonidal Cyst: This type of boil forms in the cleft of the buttocks, near the tailbone. Pilonidal cysts are often associated with ingrown hairs and can be recurrent.
- Hidradenitis Suppurativa: Hidradenitis suppurativa is a chronic skin condition characterized by the formation of multiple interconnected boils in areas with sweat glands, such as the armpits, groin, and buttocks.
Boils, while often uncomfortable and painful, are typically manageable with proper care and hygiene. Understanding the symptoms and causes of boils is essential for early detection and appropriate treatment. Maintaining good personal hygiene, avoiding skin trauma, and addressing any underlying health conditions are crucial steps in preventing the occurrence of boils.
It’s essential to note that individuals with weakened immune systems or chronic skin conditions may be more prone to recurrent boils and should work closely with healthcare providers to manage their condition effectively.
Callosities (corns)

Callosities (corns)
Callosities, also known as calluses, are thickened and hardened areas of the skin that develop in response to repeated friction, pressure, or irritation. They commonly form on the hands and feet, providing a protective layer against excessive wear and tear. While calluses are generally harmless, they can sometimes cause discomfort or pain. Understanding the symptoms, causes, and types of callosities is important for proper management.
Symptoms:
- Thickened Skin: Callosities are characterized by areas of skin that become thickened and tough.
- Hardened Bumps: The affected skin may develop raised, hardened bumps or patches.
- Discoloration: Calluses can appear yellowish or grayish in color.
- Pain or Tenderness: In some cases, callosities may cause pain or tenderness, especially when pressure is applied.
Causes:
- Friction or Pressure: The primary cause of callosities is repeated friction or pressure on a specific area of the skin. This often occurs due to activities like walking or running, or from wearing ill-fitting shoes.
- Poorly Fitted Footwear: Shoes that are too tight or do not provide proper support can lead to increased friction, causing callosities to form on the feet.
- Manual Labor or Tools: People engaged in manual labor or activities involving hand tools may develop callosities on their hands due to constant pressure or rubbing.
- Musical Instruments: Musicians who play instruments that require extensive hand use, such as string instruments or the guitar, may develop callosities on their fingertips.
- Abnormalities in Foot Structure: Conditions like bunions or hammertoes can cause increased pressure on specific areas of the foot, leading to the formation of callosities.
- Aging: As skin ages, it may lose some of its natural elasticity, making it more prone to developing calluses.
- Inflammatory Skin Conditions: Certain skin conditions, such as eczema or psoriasis, can contribute to the development of callosities.
Types:
- Plantar Calluses: These develop on the soles of the feet, often near the ball or heel, due to pressure from walking or standing.
- Palmar Calluses: Form on the palms of the hands and are commonly seen in individuals engaged in manual labor or activities involving tools.
- Focal Calluses: Occur at specific points on the skin and are typically smaller in size.
- Peripheral Calluses: Develop at the edges of the hands and feet and may result from abnormal weight distribution or friction.
Carbuncle

Carbuncle
A carbuncle is a painful, localized collection of multiple connected boils (furuncles) that form a cluster under the skin. Boils and carbuncles are skin infections that result from the invasion of bacteria, usually Staphylococcus aureus, into hair follicles. Carbuncles can develop anywhere on the body but are commonly found on the back of the neck, shoulders, thighs, and buttocks. Understanding the symptoms, causes, and types of carbuncles is important for proper diagnosis and treatment.
Symptoms:
- Pain and Tenderness: Carbuncles are typically painful, and the affected area can be tender to the touch.
- Red, Swollen Bumps: The skin around the carbuncle becomes red, swollen, and may feel warm.
- Pus Drainage: As the carbuncle progresses, it may develop a center filled with pus that eventually drains out.
- 4. Fever and Fatigue: In some cases, individuals may experience systemic symptoms, including fever and fatigue.
Causes:
- Bacterial Infection: Carbuncles result from a bacterial infection, primarily by Staphylococcus aureus. The bacteria enter the skin through small cuts or hair follicles, leading to the formation of a cluster of boils.
- Weakened Immune System: People with weakened immune systems, diabetes, or other underlying health conditions may be more susceptible to developing carbuncles.
- Poor Hygiene: Lack of proper hygiene can contribute to the development and spread of bacterial infections on the skin.
- Close Contact: Sharing personal items, such as towels or razors, with an infected individual can increase the risk of developing carbuncles.
Types:
- Single Carbuncle: This is a single, large cluster of boils, often characterized by a central core containing pus.
- Recurrent Carbuncles: Some individuals may experience multiple episodes of carbuncles, indicating a tendency for recurrent skin infections.
- Occupational Carbuncles: Certain professions that involve exposure to environmental factors, such as dust or chemicals, may increase the risk of developing carbuncles.
Cellulitis

Cellulitis
Cellulitis is a bacterial skin infection that affects the deeper layers of the skin and subcutaneous tissues. It is usually caused by bacteria entering the skin through a break or crack, leading to inflammation and infection. Cellulitis can occur anywhere on the body but is most common in the lower legs. Understanding its symptoms, causes, and types is essential for proper diagnosis and treatment.
Symptoms:
- Redness and Swelling: The affected area becomes red, swollen, and may feel warm to the touch.
- Pain and Tenderness: Pain or tenderness often accompanies cellulitis, especially with pressure on the affected area.
- Skin Changes: The skin may develop a glossy appearance and may be stretched, with a possible peau d’orange texture.
- Fever and Chills: Systemic symptoms such as fever and chills may occur, indicating a more severe infection.
- Blisters or Pus Formation: In some cases, blisters or areas of pus may develop, indicating the presence of bacterial infection.
Causes:
- Bacterial Infection: The most common cause of cellulitis is infection with bacteria, primarily Streptococcus or Staphylococcus species.
- Skin Breaks or Cuts: Bacteria enter the skin through cuts, wounds, insect bites, or other breaks in the skin’s protective barrier.
- Pre-existing Skin Conditions: Skin conditions like eczema or dermatitis, which compromise the integrity of the skin, can increase the risk of cellulitis.
- Weakened Immune System: Individuals with weakened immune systems, due to conditions such as diabetes or HIV, are more susceptible to infections.
- Lymphedema: Impaired lymphatic drainage, as seen in conditions like lymphedema, can predispose individuals to cellulitis.
Types:
- Facial Cellulitis: Infection occurring on the face, particularly around the eyes and cheeks.
- Periorbital Cellulitis: Involving the tissues around the eye, often affecting children.
- Hand Cellulitis: Affecting the hands and fingers, often associated with finger injuries or hangnails.
- Perianal Cellulitis: Occurring in the anal region, sometimes associated with conditions like perianal abscess.
- Lower Leg Cellulitis: The most common type, often affecting the lower legs, particularly in individuals with venous insufficiency or edema.
Cold Sores (Fever Blisters)

Cold Sores (Fever Blisters)
Cold sores, also known as fever blisters, are small, painful, fluid-filled lesions that typically appear on or around the lips, although they can occur in other areas of the face or inside the mouth. They are caused by the herpes simplex virus (HSV), with the most common types being HSV-1 and, less commonly, HSV-2. Understanding the symptoms, causes, and types of cold sores can help in managing and preventing outbreaks.
Symptoms:
- Tingling or Itching: Before the appearance of the physical sore, individuals may experience tingling or itching at the site.
- Small Blisters: Clusters of small, fluid-filled blisters develop, often surrounded by redness.
- Pain or Discomfort: Cold sores can be painful, especially during the initial outbreak.
- Ulceration: The blisters may burst, leaving open sores or ulcers.
- Crusting and Scabbing: As the sores begin to heal, they may crust over and form scabs.
- Duration: Cold sores typically resolve within a couple of weeks, with the initial outbreak being more prolonged than subsequent episodes.
Causes:
- Herpes Simplex Virus (HSV): HSV, particularly HSV-1, is the primary cause of cold sores. It is highly contagious and can be transmitted through direct contact with the fluid from cold sores or through oral secretions.
- Initial Infection: Many individuals contract HSV during childhood or adolescence, often through non-sexual contact, such as sharing utensils or receiving a kiss from a family member with an active outbreak.
- Reactivation: After the initial infection, the virus remains dormant in nerve cells. Stress, illness, sun exposure, hormonal changes, or a weakened immune system can trigger viral reactivation, leading to recurrent cold sores.
Types:
- Primary Infection: The first exposure to HSV, often occurring during childhood, can result in a more prolonged and severe outbreak with flu-like symptoms. After the initial infection, the virus establishes latency in nerve cells.
- Recurrent Outbreaks: Subsequent outbreaks tend to be milder than the initial infection. Triggers such as stress, illness, or sun exposure can prompt the virus to reactivate, leading to the recurrence of cold sores.
- Asymptomatic Shedding: Some individuals may carry the virus without experiencing noticeable symptoms. However, they can still shed the virus and potentially transmit it to others, even in the absence of visible sores.
While there is no cure for HSV, antiviral medications and preventive measures can effectively manage cold sores, reduce symptoms, and minimize the frequency of outbreaks. Individuals with frequent or severe outbreaks should consult a healthcare professional for personalized treatment and management strategies.
Contact Dermatitis

Contact Dermatitis
Contact dermatitis is a skin condition characterized by inflammation of the skin due to direct contact with a substance that triggers an allergic or irritant reaction. This can result in a range of symptoms, from redness and itching to blistering and swelling. Understanding the symptoms, causes, and types of contact dermatitis is essential for effective management and prevention.
Symptoms:
- Red Rash: The skin affected by contact dermatitis typically develops a red rash.
- Itching: Itching is a common symptom and can range from mild to severe.
- Blistering: In some cases, the affected skin may develop blisters filled with fluid.
- Swelling: Swelling of the skin may occur, contributing to discomfort.
- Dry, Cracked Skin: Prolonged irritation can lead to dryness and cracking of the skin.
- Burning Sensation: Some individuals may experience a burning or stinging sensation.
- Oozing or Weeping: Severe cases may involve oozing or weeping of fluid from the affected skin.
Causes:
- Allergic Contact Dermatitis: This type occurs when the skin comes into contact with a substance to which the individual is allergic. Common allergens include certain metals (e.g., nickel), fragrances, preservatives, or plants like poison ivy.
- Irritant Contact Dermatitis: Caused by direct irritation of the skin, irritant contact dermatitis can result from exposure to harsh chemicals, detergents, acids, or prolonged contact with water.
- Occupational Exposures: Certain professions, such as healthcare, cleaning, or hairdressing, may involve repeated exposure to irritants or allergens, increasing the risk of contact dermatitis.
- Personal Care Products: Ingredients in cosmetics, lotions, or skincare products can trigger allergic reactions.
- Medications: Certain topical medications or antibiotics applied to the skin may lead to contact dermatitis in sensitive individuals.
Types:
- Allergic Contact Dermatitis: Triggered by an immune response to an allergen, allergic contact dermatitis often develops 24 to 48 hours after exposure. Common allergens include metals, fragrances, latex, and certain plants.
- Irritant Contact Dermatitis: Caused by direct irritation of the skin, irritant contact dermatitis can result from exposure to acids, alkalis, detergents, or other harsh substances. Symptoms can develop rapidly after exposure.
- Occupational Contact Dermatitis: Individuals in specific professions may be at higher risk due to regular exposure to irritants or allergens in the workplace.
- Photocontact Dermatitis: This type involves a reaction triggered by exposure to sunlight (UV radiation) after contact with certain substances, including some medications or plant compounds.
Dandruff / Scaling of the Scalp
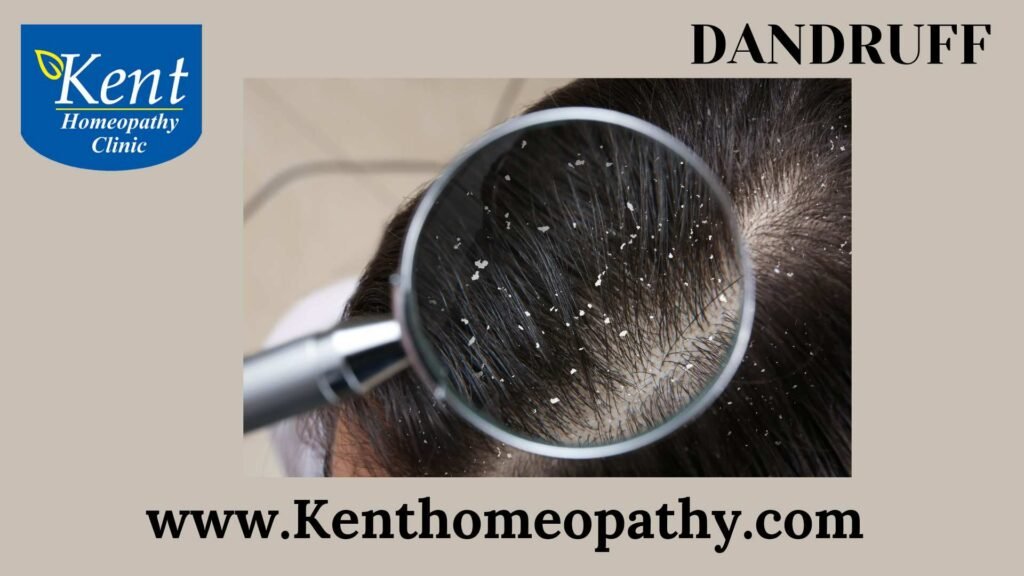
Dandruff / Scaling of the Scalp
Dandruff is a common scalp condition characterized by the shedding of small, white flakes of dead skin. While it is usually harmless, dandruff can be bothersome and may lead to self-consciousness. Understanding the symptoms, causes, and types of dandruff is essential for effective management.
Symptoms:
- White Flakes: The most noticeable symptom is the presence of white, oily or dry flakes on the scalp and in the hair.
- Itchy Scalp: Dandruff is often accompanied by an itchy scalp, which can lead to scratching.
- Redness: Scratching the scalp may cause irritation and redness.
- Oily Scalp: In some cases, dandruff is associated with an oily or greasy scalp.
Causes:
- Malassezia Yeast: The most common cause of dandruff is the overgrowth of a yeast-like fungus called Malassezia. This fungus is naturally present on the scalp but can proliferate, leading to increased skin cell turnover and flaking.
- 2. Dry Skin: Dry skin on the scalp can result in small, dry flakes that resemble dandruff.
- Seborrheic Dermatitis: A more severe form of dandruff, seborrheic dermatitis involves red, inflamed skin and greasy, yellowish scales. It often affects areas with more oil glands, including the scalp, face, and chest.
- Not Cleaning Hair Regularly: Infrequent shampooing can lead to the accumulation of oil and dead skin cells on the scalp, contributing to dandruff.
- Sensitive Skin: Individuals with sensitive skin may be more prone to developing dandruff.
- Certain Hair Care Products: The use of hair care products that irritate the scalp or trigger an allergic reaction can contribute to dandruff.
- Medical Conditions: Certain medical conditions, such as psoriasis or eczema, can lead to dandruff-like symptoms.
Types:
- Dry Skin-Related Dandruff: Often characterized by small, dry flakes, this type is associated with insufficient moisture on the scalp.
- Oily Scalp-Related Dandruff: In this type, large, oily flakes may be present, and the scalp tends to be greasier. It is associated with the overproduction of oil and the presence of Malassezia yeast.
- Seborrheic Dermatitis: This form of dandruff involves red, inflamed skin, and greasy, yellowish scales. It may extend beyond the scalp to other oily areas like the face and chest.
It’s essential to choose a dandruff treatment based on the specific cause, and individuals with persistent or severe symptoms should consult with a healthcare professional for personalized recommendations. Maintaining good scalp hygiene and addressing underlying causes can significantly reduce dandruff symptoms.
Dermatology

Dermatology
Dermatology is a branch of medicine focused on the study, diagnosis, and treatment of conditions related to the skin, hair, nails, and mucous membranes. Dermatologists are medical professionals specialized in managing a broad range of skin-related issues. Understanding the symptoms, causes, and types of dermatological conditions is crucial for effective dermatologic care.
Symptoms of Dermatological Conditions:
- Rashes: Changes in the skin’s color, texture, or appearance, often accompanied by itching.
- Lesions: Abnormal growths, lumps, or bumps on the skin.
- Itching or Pruritus: Persistent itching, which can be a symptom of various skin disorders.
- Redness or Inflammation: Increased blood flow to a particular area, leading to redness and swelling.
- Pain or Discomfort: Skin conditions may cause pain or discomfort, ranging from mild to severe.
- Changes in Pigmentation: Altered skin color, including hyperpigmentation (darkening) or hypopigmentation (lightening).
- Scaling or Peeling: Shedding of the outer layer of the skin, often seen in conditions like psoriasis.
- Ulcers or Sores: Openings or breaks in the skin surface, which can be indicative of various dermatologic issues.
Causes of Dermatological Conditions:
- Infections: Bacterial, viral, or fungal infections can affect the skin, causing conditions like acne, warts, or fungal infections.
- Genetic Factors: Some skin conditions have a genetic predisposition, such as psoriasis or eczema.
- Autoimmune Disorders: Conditions like lupus or pemphigus involve the immune system attacking the skin.
- Environmental Factors: Exposure to certain substances or environmental factors can lead to skin issues, including contact dermatitis.
- Allergies: Allergic reactions to substances like plants, chemicals, or medications can manifest as skin conditions.
- Hormonal Changes: Fluctuations in hormones, as seen in conditions like acne or melasma.
- Trauma or Injury: Burns, cuts, or other injuries can result in dermatological problems, including scarring.
- Malignancies: Skin cancers, such as melanoma or basal cell carcinoma, are forms of malignancies that affect the skin.
Types of Dermatological Conditions:
- Acne: A common skin condition characterized by the formation of pimples, blackheads, and whiteheads.
- Eczema (Dermatitis): Inflammation of the skin leading to redness, itching, and scaling.
- Psoriasis: An autoimmune condition causing the rapid buildup of skin cells, resulting in thick, scaly patches.
- Rosacea: Chronic skin condition leading to redness, flushing, and visible blood vessels on the face.
- Skin Cancer: Various forms of skin cancer, including melanoma, squamous cell carcinoma, and basal cell carcinoma.
- Fungal Infections: Infections caused by fungi, such as ringworm or athlete’s foot.
- Vitiligo: Loss of skin color due to the destruction of pigment-producing cells.
- Hives (Urticaria): Raised, red, itchy welts on the skin often triggered by allergies.
Diaper Rash

Diaper Rash
Diaper rash is a common skin irritation that occurs in the diaper-covered area of infants and toddlers. It typically manifests as red, inflamed skin and can be uncomfortable for the child. Understanding the symptoms, causes, and types of diaper rash is essential for effective prevention and management.
Symptoms:
- Redness: The affected area appears red and irritated, often extending beyond the diaper area.
- Inflammation: Swelling and tenderness may accompany the redness.
- Warmth: The skin may feel warm to the touch.
- Papules or Pustules: Small, raised bumps (papules) or fluid-filled lesions (pustules) may develop.
- Peeling or Flaking: The affected skin may peel or flake, indicating skin damage.
- Discomfort: Infants with diaper rash may seem irritable or uncomfortable, especially during diaper changes.
Causes:
- Prolonged Exposure to Moisture: Wet diapers, whether from urine or stool, can soften the skin and make it more susceptible to irritation.
- Friction: Rubbing or chafing from the diaper against the skin can contribute to diaper rash.
- Infrequent Diaper Changes: Not changing diapers promptly allows moisture and irritants to remain in contact with the skin.
- New Foods or Medications: Introducing new foods or medications, especially for breastfed babies or those starting solid foods, can lead to changes in stool consistency, potentially causing diaper rash.
- Bacterial or Fungal Infections: Candida, a yeast-like fungus, can thrive in the warm, moist environment of a diaper and contribute to diaper rash.
- Sensitive Skin: Some babies have more sensitive skin, making them prone to diaper rash.
Types:
- Contact Dermatitis: This is the most common type of diaper rash and is caused by prolonged exposure to wetness, friction, or irritants in diapers.
- Yeast (Candida) Infection: Candida diaper rash is characterized by bright red skin, often with red or scaly borders. It may involve the folds and creases of the skin.
- Bacterial Infection: A bacterial infection can occur when the skin is compromised, leading to pustules, crusting, or oozing.
- Allergic Reaction: Some babies may develop an allergic reaction to certain diaper materials, wipes, or creams, resulting in a rash.
If diaper rash persists or worsens despite home care measures, or if there are signs of infection (such as oozing, pus, or fever), it’s important to consult with a healthcare professional for further evaluation and appropriate treatment. Diaper rash is a common concern, and with proper care and preventive measures, it can often be effectively managed.
Dry Skin Disease (Icthyosis)

Dry Skin Disease (Icthyosis)
Dry skin, is a common skin condition characterized by a lack of moisture and a compromised skin barrier. This condition can affect individuals of all ages and is influenced by various factors, including environmental conditions, genetics, and lifestyle choices.
Symptoms:
- Itching: Dry skin is often accompanied by itching, which can be mild to severe.
- Flaking or Peeling: The skin may appear flaky or peel, especially in areas prone to dryness.
- Redness: Dry skin can lead to red patches, and in some cases, the skin may crack or develop fine lines.
- Tightness: The affected skin may feel tight or uncomfortable, particularly after bathing.
Causes:
- Environmental Factors: Exposure to harsh weather conditions, low humidity, or excessive sun and wind can strip the skin of its natural oils, contributing to dryness.
- Hot Showers and Bathing Habits: Long, hot showers or baths can remove the skin’s natural oils, leading to dryness.
- Age: Aging is associated with a decline in oil production, making older individuals more prone to dry skin.
- Genetics: Some people may have a genetic predisposition to dry skin, with a natural tendency for their skin to produce fewer oils.
- Skin Conditions: Certain skin conditions, such as eczema (atopic dermatitis) and psoriasis, can cause dryness and exacerbate symptoms.
Types:
- Asteatotic Eczema: Also known as “winter itch,” it is characterized by dry, cracked, and itchy skin, often occurring in older individuals during the winter months.
- Contact Dermatitis: Exposure to irritants or allergens can lead to dry, red, and itchy skin in localized areas.
- Ichthyosis: This genetic condition results in the formation of thick, dry, fish-like scales on the skin’s surface.
- Xerosis: Generalized dry skin without any underlying skin condition is referred to as xerosis. It often worsens in dry climate.
For persistent or severe cases, it’s advisable to seek advice from a dermatologist who can provide a more personalized approach to managing dry skin and address any underlying skin conditions contributing to the problem.
Eczema

Eczema
Eczema, also known as atopic dermatitis, is a chronic inflammatory skin condition characterized by red, itchy, and inflamed skin. It often begins in childhood but can affect individuals of any age. Eczema is not contagious, and while there is no cure, various treatments can help manage symptoms.
Symptoms:
- Itching: Intense itching is a hallmark symptom of eczema, and scratching can worsen the condition.
- Red or Inflamed Skin: Areas of the skin affected by eczema may appear red, swollen, and inflamed.
- Dry or Cracked Skin: The affected skin often becomes dry, and in severe cases, it may crack, leading to increased vulnerability to infections.
- Blisters or Oozing Lesions: In some cases, eczema can cause the formation of small blisters or oozing lesions, especially during flare-ups.
- Thickened Skin: Prolonged scratching or rubbing can lead to thickened, leathery skin, known as lichenification.
Causes:
- Genetics: There is a strong genetic component to eczema, and individuals with a family history of atopic conditions (eczema, asthma, hay fever) are more predisposed.
- Immune System Dysfunction: Eczema is linked to an overactive immune response, causing inflammation in the skin.
- Environmental Triggers: Exposure to irritants such as harsh soaps, detergents, or certain fabrics can exacerbate eczema symptoms.
- Allergens: Allergens like pollen, dust mites, pet dander, or certain foods can trigger or worsen eczema in some individuals.
- Skin Barrier Dysfunction: Individuals with eczema often have a compromised skin barrier, allowing irritants to penetrate more easily and moisture to escape, leading to dryness.
Types:
- Atopic Dermatitis: The most common form of eczema, atopic dermatitis often begins in childhood and is associated with a family history of atopic conditions.
- Contact Dermatitis: This type is triggered by contact with irritants or allergens. It can be further classified into irritant contact dermatitis and allergic contact dermatitis.
- Nummular Eczema: Characterized by coin-shaped patches of irritated skin, nummular eczema may be linked to dry skin and environmental factors.
- Seborrheic Dermatitis: Often affecting the scalp and face, seborrheic dermatitis is associated with red, scaly, and oily skin. It can occur in infants as cradle cap.
- Dyshidrotic Eczema: This type involves the formation of small, itchy blisters on the hands and feet, and is often triggered by stress or exposure to certain metals.
Individuals with eczema should work closely with dermatologists to develop a personalized treatment plan. While there is no cure, effective management strategies can significantly improve the quality of life for those with eczema.
Erysipelas

Erysipelas
Erysipelas is a bacterial skin infection caused primarily by Streptococcus pyogenes, also known as group A Streptococcus. This infection affects the superficial layers of the skin and underlying tissues, leading to characteristic symptoms and a distinctive appearance. Erysipelas requires prompt medical attention for appropriate treatment.
Symptoms:
- Skin Redness: Erysipelas typically presents as a well-defined area of bright red, swollen skin with a raised border.
- Pain and Tenderness: The affected area is often tender to the touch and may be accompanied by pain.
- Fever: Erysipelas is frequently associated with systemic symptoms, including fever and chills.
- Swelling: Swelling of the affected area is common, contributing to the characteristic appearance.
- Blisters or Pustules: In severe cases, blisters or pustules may form on the affected skin.
Causes:
- 1. Streptococcus pyogenes Infection: Erysipelas is most commonly caused by infection with Streptococcus pyogenes bacteria. The bacteria enter the skin through cuts, wounds, or areas of compromised skin integrity.
- Risk Factors:
– Skin Breaks or Injuries: Any break in the skin, such as cuts, abrasions, or surgical wounds, can provide an entry point for bacteria.
– Impaired Lymphatic Drainage: Conditions that affect the lymphatic system, such as chronic edema or lymphedema, can increase the risk.
– Weakened Immune System: Individuals with compromised immune systems are more susceptible to bacterial infections.
Types:
- Facial Erysipelas: The face, particularly around the eyes, nose, and cheeks, is a common site for erysipelas.
- Leg Erysipelas: Involves the lower extremities, especially the shin and calf areas. Leg erysipelas is a frequent occurrence.
- Other Body Areas: While facial and leg erysipelas are most common, the infection can occur on other body parts.
Complications:
- Abscess Formation: In some cases, abscesses may develop within the affected skin.
- Cellulitis: Erysipelas can lead to cellulitis, a deeper skin infection.
- Systemic Spread: While rare, severe cases may lead to bloodstream infections (bacteremia) or other complications.
Prompt diagnosis and initiation of appropriate antibiotic treatment are crucial for a favorable outcome in erysipelas. Individuals with symptoms suggestive of this infection, especially if associated with fever, should seek medical attention for timely evaluation and management. Adherence to prescribed antibiotic regimens and close follow-up with healthcare providers are essential for successful recovery.
Fungal infection

Fungal infection
Fungal Infection:
Fungal infections, also known as mycoses, are caused by various types of fungi and can affect different parts of the body. These infections can range from mild to severe, and symptoms may vary based on the type of fungus and the affected area.
Symptoms:
- Skin Infections:
– Itching and redness on the skin.
– Formation of rashes or blisters.
– Peeling or cracking of the skin.
– Fungal infections like athlete’s foot or ringworm commonly affect the skin.
- Nail Infections:
– Thickening, discoloration, or deformation of nails.
– Brittle or crumbly nails.
– Fungal nail infections often affect toenails and fingernails.
- Oral Infections:
– White patches in the mouth or on the tongue (oral thrush).
– Soreness and difficulty swallowing.
– Fungal infections like candidiasis can impact the mouth and throat.
- Genital Infections:
– Itching, redness, and discomfort in the genital area.
– Abnormal vaginal discharge in women.
– Fungal infections like yeast infections commonly affect the genital region.
- Systemic Infections:
– Fever and chills.
– Respiratory symptoms if the infection spreads to the lungs.
– Systemic fungal infections can be severe and affect internal organs.
Causes:
- Fungal Species: Different fungi, including yeasts and molds, can cause infections. Common culprits include Candida, Aspergillus, and dermatophytes.
- Weakened Immune System: Individuals with compromised immune systems, such as those with HIV/AIDS or undergoing immunosuppressive therapy, are more susceptible to fungal infections.
- Environmental Exposure: Fungi thrive in warm and humid environments. Exposure to contaminated soil, water, or surfaces can contribute to infections.
- Poor Hygiene: Lack of proper hygiene, especially in moist areas like skin folds, can create an environment conducive to fungal growth.
- Use of Antibiotics: Prolonged use of antibiotics can disrupt the balance of microorganisms in the body, allowing fungi to proliferate.
Types:
- Superficial Infections:
– Cutaneous Infections: Affect the skin, hair, or nails. Examples include athlete’s foot, ringworm, and nail infections.
– Mucocutaneous Infections: Involve both the skin and mucous membranes, such as oral thrush.
- Subcutaneous Infections:
– Extend into the deeper layers of the skin and tissues. These infections are less common and may result from traumatic injuries. Examples include sporotrichosis.
- Systemic Infections:
– Involve internal organs and can be life-threatening. Examples include invasive candidiasis and aspergillosis.
- Opportunistic Infections:
– Occur in individuals with weakened immune systems. Fungi that are normally harmless can cause infections in these cases. Examples include cryptococcosis in HIV/AIDS patients.
Herpes Zoster (Shingles)

Herpes Zoster (Shingles)
Herpes Zoster (Shingles): Understanding Symptoms, Causes, and Types
Herpes Zoster, commonly known as shingles, is a viral infection caused by the reactivation of the varicella-zoster virus, which is responsible for chickenpox. After a person has had chickenpox, the virus can remain dormant in nerve cells and later re-emerge as shingles. Understanding the symptoms, causes, and types of herpes zoster is essential for accurate diagnosis and appropriate management.
Symptoms:
- Pain and Tingling: Often, the first symptom is pain or tingling in a specific area, commonly on one side of the body or face.
- Rash: A rash typically follows the pain, developing into red, fluid-filled blisters that resemble a band or strip. The rash is usually limited to one side of the body.
- Itching: The affected area may be intensely itchy.
- Flu-Like Symptoms: Some individuals may experience fever, headache, and general malaise.
- Sensitivity to Touch: The rash and affected skin can be sensitive to touch.
Causes:
The primary cause of herpes zoster is the reactivation of the varicella-zoster virus, which remains dormant in nerve cells after a person has had chickenpox. Several factors may contribute to the reactivation, including:
- Weakened Immune System: Conditions such as aging, immunosuppressive medications, or diseases like HIV can weaken the immune system, allowing the virus to resurface.
- Stress: Physical or emotional stress may trigger the reactivation of the virus.
- Certain Medications: Some medications, particularly those affecting the immune system, may increase the risk of shingles.
Types:
- Dermatomal Shingles: The most common type, affecting a specific dermatome (area of skin) served by a single nerve or nerve group. This often results in a band-like pattern of rash on one side of the body.
- Ophthalmic Shingles: Involves the nerves around the eye, potentially causing eye pain, redness, and vision problems.
- Ramsay Hunt Syndrome: Affects the facial nerve, leading to ear pain, rash around the ear, and facial weakness.
- Disseminated Shingles: In rare cases, the rash can spread to a larger area or involve multiple dermatomes, posing a greater risk of complications.
HFMD

HFMD
Hand, Foot, and Mouth Disease (HFMD): Understanding Symptoms, Causes, and Types
Hand, Foot, and Mouth Disease (HFMD) is a viral illness primarily affecting infants and children, although it can also occur in adults. It is commonly caused by enteroviruses, with the most prevalent culprits being coxsackieviruses, particularly Enterovirus 71 and Coxsackievirus A16. Understanding the symptoms, causes, and types of HFMD is crucial for early detection and appropriate management.
Symptoms:
- Fever: HFMD often begins with a sudden onset of fever, which may be moderate to high.
- Sore Throat: Painful sores or ulcers may develop in the mouth, leading to discomfort and difficulty swallowing.
- Rash: Small, red spots or blisters may appear on the palms of the hands, soles of the feet, and sometimes on the knees, elbows, or buttocks.
- Loss of Appetite: Children with HFMD may experience a reduced desire to eat due to soreness in the mouth.
- Irritability: Young children may become irritable or fussy, especially if they are experiencing pain from mouth sores.
Causes:
HFMD is primarily caused by enteroviruses, and transmission occurs through:
- Close Contact: The virus spreads through respiratory droplets from an infected person, such as coughing or sneezing.
- Contact with Contaminated Surfaces: Touching surfaces or objects contaminated with the virus and then touching the face, mouth, or hands.
- Fecal-Oral Route: In some cases, the virus may be present in the feces of an infected person, leading to transmission through contaminated food, water, or surfaces.
Types:
While coxsackieviruses, particularly A16 and Enterovirus 71, are the primary causes of HFMD, there can be variations in symptoms and severity. Enterovirus 71, in particular, is associated with more severe cases, including neurological complications. Coxsackievirus A6 has also been linked to more atypical and severe presentations of HFMD.
Complications:
While HFMD is typically a mild and self-limiting illness, complications may occur, especially in severe cases. These complications can include:
- Dehydration: Difficulty in eating and drinking due to mouth sores can lead to dehydration, especially in young children.
- Secondary Infections: Bacterial infections may occur if the blisters become scratched or infected.
- Neurological Complications: Enterovirus 71, in rare cases, has been associated with neurological complications such as encephalitis, which can be serious.
Hidradenitis suppurative

Hidradenitis suppurative
Hidradenitis Suppurativa (HS): Understanding Symptoms, Causes, and Types
Hidradenitis Suppurativa (HS) is a chronic skin condition characterized by the formation of painful, inflamed bumps or abscesses, typically in areas where skin rubs together, such as the armpits, groin, buttocks, and under the breasts. HS is often associated with the inflammation of hair follicles and can lead to the development of tunnels connecting the abscesses under the skin. Understanding the symptoms, causes, and types of HS is crucial for effective management.
Symptoms:
- Painful Bumps: The primary symptom is the formation of painful, swollen bumps or nodules under the skin, which may rupture and release pus.
- Tunnels (Sinus Tracts): Over time, tunnels or channels under the skin (sinus tracts) may develop, connecting the affected areas.
- Scar Formation: Repeated flare-ups can lead to the formation of scar tissue, resulting in thickened, rope-like scars.
- Itching: Itching and burning sensations may be experienced in the affected areas.
- Malodorous Discharge: In some cases, the abscesses may release a foul-smelling discharge.
Causes:
The exact cause of HS is not fully understood, but several factors contribute to its development:
- Genetic Predisposition: There appears to be a genetic component, as HS often occurs in individuals with a family history of the condition.
- Inflammation: Chronic inflammation in the hair follicles and sweat glands is a key factor, leading to the formation of abscesses and tunnels.
- Obesity: Excess weight and obesity are associated with an increased risk of HS, possibly due to friction and sweat accumulation in skin folds.
- Smoking: Smoking has been linked to a higher prevalence and severity of HS.
- Hormonal Factors: Hormonal changes may play a role, as HS often begins after puberty and may worsen with hormonal fluctuations.
- Immune System Dysfunction: An abnormal immune response may contribute to the inflammation seen in HS.
Types:
HS is classified into three stages based on severity:
- Stage I (Hurley Stage I):
Characterized by the presence of single or multiple isolated abscesses without significant scarring or sinus tracts.
- Stage II (Hurley Stage II):
In this stage, recurrent abscesses, sinus tracts, and scarring are evident, often occurring in multiple areas.
- Stage III (Hurley Stage III):
Advanced stage with widespread involvement, multiple interconnected sinus tracts, and severe scarring. This stage may significantly impact daily life and function.
Ichthyosis

Ichthyosis
Ichthyosis refers to a group of genetic skin disorders characterized by dry, scaly skin. These conditions result from a dysfunction in the skin’s natural shedding process, leading to the accumulation of skin cells. Here’s an overview of ichthyosis, including its symptoms, causes, and types:
Symptoms of Ichthyosis:
- Dry, Scaly Skin:
– The hallmark symptom of ichthyosis is the presence of dry, scaly skin. The scales may range from fine to thick, and their appearance can vary depending on the specific type of ichthyosis.
- Itching:
– Many individuals with ichthyosis experience itching, which can be mild to severe and may contribute to skin irritation.
- Cracked Skin:
– The skin affected by ichthyosis is prone to cracking, especially in areas that experience friction or pressure.
- Redness:
– The affected skin may appear red or inflamed due to the dryness and scaling.
- Pain and Discomfort:
– In severe cases, ichthyosis can cause pain and discomfort, especially if the skin becomes tight and rigid.
- Restricted Movement:
– In some forms of ichthyosis, the skin’s tightness and scaling can limit joint movement and flexibility.
- Increased Susceptibility to Infections:
– The compromised skin barrier in ichthyosis can make individuals more prone to skin infections.
- Eye Involvement:
– In some types, the scales may extend to the eyelids and cause irritation or restrict eye movement.
Causes of Ichthyosis:
- Genetic Mutations:
– The majority of ichthyosis cases are inherited and result from genetic mutations. The specific genes involved vary depending on the type of ichthyosis.
- Autosomal Dominant Inheritance:
– Some types of ichthyosis follow an autosomal dominant pattern, meaning an affected individual has a 50% chance of passing the condition to their offspring.
- Autosomal Recessive Inheritance:
– Other types are inherited in an autosomal recessive manner, requiring both parents to carry the mutated gene for a child to be affected.
- Acquired Ichthyosis:
– While rare, ichthyosis can develop later in life due to certain medical conditions, such as hypothyroidism, lymphoma, or the use of certain medications.
Types of Ichthyosis:
- Ichthyosis Vulgaris:
– The most common type, typically appearing in childhood. It often improves with age but may persist into adulthood.
- X-Linked Ichthyosis:
– Affects males more severely due to a mutation on the X chromosome. Females may be carriers with milder symptoms.
- Lamellar Ichthyosis:
– Presents at birth with a collodion membrane, which sheds to reveal large, dark scales. It tends to be more severe and persistent.
- Harlequin Ichthyosis:
– A severe and rare form characterized by thick, diamond-shaped plates of skin. Infants born with harlequin ichthyosis have distinct facial features and require intensive care.
- Congenital Ichthyosiform Erythroderma (CIE):
– Presents at birth with red, scaling skin. It may improve with age but often requires ongoing management.
- Netherton Syndrome:
– A rare genetic disorder associated with ichthyosis, hair abnormalities, and a predisposition to allergies and infections.
- Ichthyosis Hystrix:
– A group of rare ichthyoses with spiky or horn-like scales. Each subtype has distinct features and genetic causes.
- Erythrokeratodermia Variabilis:
– Characterized by variable red patches and scaling. Symptoms may fluctuate throughout life.
- Acquired Ichthyosis:
– Develops later in life and is often associated with underlying medical conditions or medications.
Impetigo

Impetigo
Impetigo is a contagious skin infection caused by bacteria, primarily Staphylococcus aureus or Streptococcus pyogenes. It is more common in children than adults and is characterized by the development of red sores or blisters on the skin, often around the nose and mouth. Understanding the symptoms, causes, and types of impetigo is crucial for accurate diagnosis and prompt treatment.
Symptoms:
- Red Sores: The primary symptom of impetigo is the presence of red sores that quickly turn into blisters. These blisters may ooze and form a yellowish-brown crust.
- Itching: The affected area may be itchy, and scratching can contribute to the spread of the infection.
- Rash: The rash associated with impetigo can be widespread, and it may start as small red spots that evolve into larger blisters.
- Fluid-filled Blisters: The blisters may contain fluid that can spread the infection to other parts of the body or to other people through direct contact.
- Honey-Colored Crusts: As the blisters rupture, they leave behind a characteristic honey-colored crust. This crust is a key feature in distinguishing impetigo from other skin conditions.
- Swollen Lymph Nodes: In some cases, nearby lymph nodes may become swollen as the body responds to the bacterial infection.
Causes:
- Bacterial Infection: Impetigo is caused by bacteria, with Staphylococcus aureus and Streptococcus pyogenes being the most common culprits. The bacteria enter the skin through cuts, scratches, or insect bites, initiating the infection.
- Poor Hygiene: Lack of proper hygiene, especially in crowded or unsanitary conditions, can increase the risk of impetigo.
- Skin Injuries: Any break in the skin, such as cuts, abrasions, or insect bites, provides an entry point for bacteria, increasing the likelihood of impetigo.
- Close Contact: Impetigo is highly contagious, and it can spread through direct skin-to-skin contact with an infected person. Sharing personal items, such as towels or razors, can also contribute to the transmission of the bacteria.
- Warm and Humid Environment: Bacteria thrive in warm and humid environments, making these conditions conducive to the development and spread of impetigo.
Types:
- Non-bullous Impetigo: This is the most common form of impetigo. It typically begins as small red sores that quickly progress to fluid-filled blisters. As the blisters rupture, they form a characteristic honey-colored crust. Non-bullous impetigo is often seen around the nose and mouth.
- Bullous Impetigo: Less common than non-bullous impetigo, this type is characterized by larger fluid-filled blisters. The blisters are more stable and less likely to rupture than in the non-bullous form. Bullous impetigo often affects the trunk, buttocks, and limbs.
- Ecthyma: This is a more severe and deeper form of impetigo. It extends into the deeper layers of the skin, causing painful, ulcerative sores. Ecthyma is more likely to result in scarring and may leave permanent marks on the skin.
Infantile eczema

Infantile eczema
Infantile Eczema: Unraveling Symptoms, Causes, and Types
Infantile eczema, also known as atopic dermatitis, is a common skin condition affecting infants and young children. Characterized by red, itchy rashes, this condition can be distressing for both infants and their parents. Understanding the symptoms, causes, and types of infantile eczema is crucial for effective management and care.
Symptoms:
- Red, Inflamed Skin: The hallmark symptom of infantile eczema is red, inflamed skin. This often appears in patches on the face, especially the cheeks and forehead, but can also affect other areas of the body.
- Itching: Intense itching is a characteristic feature. While infants may not be able to express their discomfort verbally, persistent scratching, fussiness, or disturbed sleep can be indicators.
- Dry and Scaly Skin: Affected areas may exhibit dryness and scaliness, leading to a rough texture on the skin surface.
- Oozing and Crusting: In severe cases, the skin may ooze clear fluid and develop crusts, especially if the affected areas are scratched repeatedly.
- Thickened Skin: Chronic scratching can result in thickened skin, known as lichenification, particularly in areas where the rash is persistent.
- Affected Areas: Common sites of involvement include the face, neck, hands, elbows, and the back of the knees. However, infantile eczema can occur on any part of the body.
Causes:
- Genetics: A family history of eczema, asthma, or allergic rhinitis increases the likelihood of an infant developing eczema. Genetic factors play a significant role in the predisposition to atopic conditions.
- Immune System Dysfunction: Infantile eczema is associated with an overactive immune response to irritants or allergens. The skin barrier in individuals with eczema may not function properly, making the skin more susceptible to inflammation.
- Environmental Factors: Exposure to environmental triggers, such as harsh soaps, detergents, or certain fabrics, can contribute to eczema flare-ups. Changes in temperature or humidity may also impact the skin.
- Allergens: Infants with eczema often have sensitivities to common allergens like certain foods, dust mites, pet dander, or pollen. Identifying and avoiding these triggers is essential in managing the condition.
- Skin Barrier Deficiency: In some cases, infants with eczema may have a compromised skin barrier that allows moisture to escape, leading to dryness and susceptibility to irritants.
- Infections: Bacterial, viral, or fungal infections can exacerbate eczema symptoms. Scratching the affected areas can create openings in the skin, providing an entry point for microbes.
Types:
- Acute Eczema: Characterized by sudden onset and intense inflammation, acute eczema often presents with red, weeping, and crusted lesions. It can be triggered by irritants or allergens.
- Subacute Eczema: This phase represents a transitional stage between acute and chronic eczema. The inflammation is less intense, and the skin may be dry, scaly, and exhibit less oozing.
- Chronic Eczema: In chronic eczema, the skin becomes thickened and lichenified due to prolonged inflammation and persistent scratching. This stage often requires ongoing management.
- Contact Dermatitis: In some cases, eczema may be triggered by contact with specific substances, leading to contact dermatitis. Identifying and avoiding these triggers is crucial in managing this type of eczema.
- Nummular Eczema: This type is characterized by coin-shaped patches of irritated skin. It can be more challenging to manage and may require specific treatment approaches.
- Seborrheic Eczema: Often seen in infants, this type primarily affects the scalp, leading to cradle cap—a condition marked by yellow, greasy scales on the scalp.
Ingrown Toenail
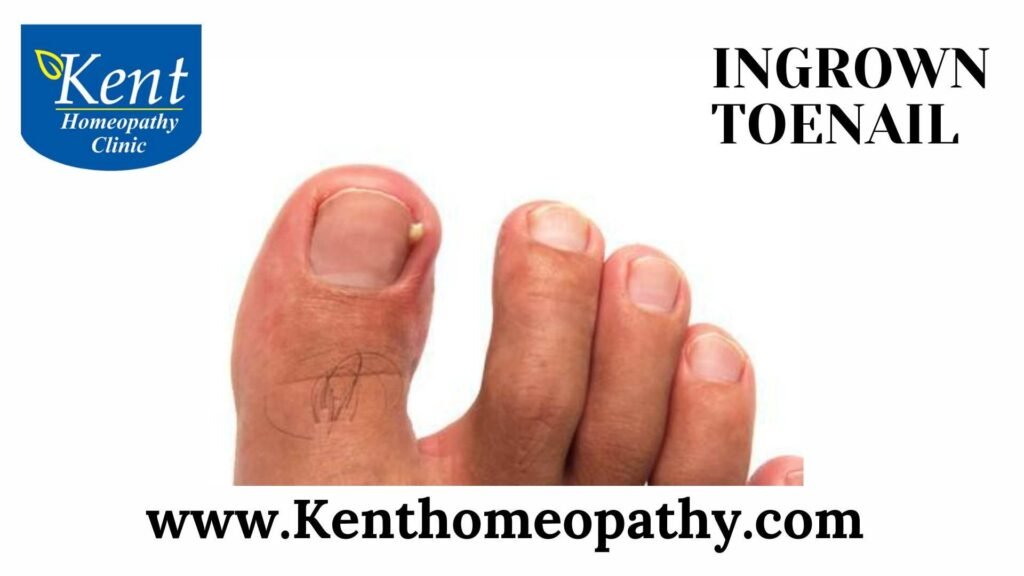
Ingrown Toenail
Ingrown Toenail: A Comprehensive Overview
An ingrown toenail is a common foot condition where the edge of a toenail, usually the one on the big toe, grows into the surrounding skin rather than over it. This can result in various symptoms, causes, and types that require attention and care.
Symptoms:
- Redness and Tenderness: In the early stages, an ingrown toenail often presents with redness and tenderness around the affected area. This is a result of the nail’s pressure against the adjacent skin.
- Swelling and Pain: As the condition progresses, swelling and pain become more pronounced. The ingrown toenail causes irritation, leading to discomfort that can be exacerbated by walking or wearing shoes.
- Pus Formation: In more advanced cases, the ingrown toenail may lead to the formation of a small, pus-filled bump. This is indicative of infection and requires attention to prevent further complications.
- Infection Symptoms: Severe cases of ingrown toenails can result in infection. Increased redness, warmth, and the drainage of yellow or green pus are signs of infection that should be addressed promptly.
Causes:
- Improper Nail Trimming: One of the primary causes of ingrown toenails is improper nail trimming. Cutting toenails too short or rounding the edges instead of trimming straight across increases the likelihood of the nail growing into the skin.
- Tight or Ill-Fitting Shoes: Footwear that is too tight or doesn’t provide enough space for toes can exert pressure on the toenails, encouraging them to grow inward.
- Genetic Predisposition: Some individuals may be genetically predisposed to ingrown toenails due to the natural shape and structure of their nails. This can make them more prone to developing this condition.
- Injuries: Trauma to the toe, such as stubbing or other injuries, can lead to irregular nail growth, increasing the risk of ingrown toenails.
- Poor Foot Hygiene: Fungal infections and inadequate foot hygiene can weaken the toenails, making them more susceptible to ingrowth.
Types:
- Ingrown Toenail without Infection: In the early stages, the toenail begins to curve and press against the surrounding skin, causing mild discomfort. This is the initial phase where intervention can prevent further complications.
- Ingrown Toenail with Infection: If left untreated, an ingrown toenail can penetrate the skin, leading to infection. Symptoms intensify, with increased pain, swelling, and the potential formation of pus.
- Chronic Ingrown Toenails: Some individuals may experience recurrent ingrown toenails due to genetic factors or underlying health conditions. These chronic cases may require ongoing management to prevent frequent occurrences.
- Ingrown Toenail with Granulation Tissue: Prolonged irritation can lead to the development of granulation tissue, a mass of new connective tissue. This tissue may appear as a reddish or pink overgrowth around the ingrown toenail, contributing to discomfort.
In conclusion, understanding ingrown toenails involves recognizing symptoms, addressing contributing factors, and adopting proper care practices. From at-home remedies to professional interventions, the approach varies based on the severity of the condition. Prompt attention and appropriate care are crucial to prevent complications and ensure effective healing.
Keloids

Keloids
Keloids: Unveiling Symptoms, Causes, and Types
Keloids are raised, overgrown scars that extend beyond the boundaries of the original injury or wound. These fibrous growths can be unsightly and, in some cases, cause discomfort or itching. Understanding the symptoms, causes, and types of keloids is essential for effective management and addressing the cosmetic and potential health concerns associated with this type of scarring.
Symptoms:
- Elevated and Raised: The primary characteristic of keloids is their raised appearance. These scars extend beyond the original wound and often have a smooth, rounded surface.
- Color Variation: Keloids can vary in color, typically appearing darker than the surrounding skin. The color may range from pink or red to dark brown.
- Itching: Keloids may be accompanied by itching or tenderness. The sensation of itching can be persistent and may contribute to discomfort.
- Growth Over Time: Unlike normal scars that gradually fade, keloids may continue to grow over time, extending beyond the initial injury site.
- Irregular Shape: Keloids often have an irregular shape and can become larger than the original wound. They may extend into surrounding healthy skin.
- Pain or Discomfort: In some cases, keloids may cause pain or discomfort, particularly if they are located in areas prone to friction or pressure.
- Contracture: Keloids on joints or areas of movement may lead to contracture, restricting movement in those regions.
Causes:
- Genetic Predisposition: There is a genetic component to keloid formation. Individuals with a family history of keloids may be more prone to developing these overgrown scars.
- Skin Type: People with darker skin tones, particularly those of African, Asian, or Hispanic descent, are more susceptible to keloid formation. However, keloids can occur in individuals of any skin type.
- Age and Gender: Keloids are more common in individuals under 30 years of age. Additionally, studies suggest that keloids may be more prevalent in women than in men.
- Wound Type: Certain types of wounds are more likely to result in keloid formation. Surgical scars, traumatic injuries, burns, acne scars, and ear piercings are common triggers.
- Hormonal Influence: Hormonal changes, particularly during puberty, pregnancy, or menopause, may contribute to keloid development.
- Tension on Wound: Excessive tension or pressure on a healing wound can increase the likelihood of keloid formation. This is more common in areas where the skin is constantly stretched or under tension.
- Inflammatory Response: An exaggerated inflammatory response to a wound or injury may contribute to the development of keloids.
- Foreign Body Reaction: In some cases, the presence of foreign materials, such as piercings or embedded debris, can trigger keloid formation.
Types:
- Hypertrophic Scars: Hypertrophic scars are similar to keloids in that they are raised and red, but they do not extend beyond the boundaries of the original wound. They tend to regress over time and may be less aggressive than keloids.
- Keloids on Earlobes: Earlobe keloids are a common type, often associated with ear piercings. These overgrown scars can be particularly challenging due to their location and potential for recurrence.
- Keloids on Chest: Keloids on the chest may result from surgical scars, acne, or other injuries in this area. The chest is prone to tension, making it susceptible to keloid formation.
- Keloids on Shoulders: Keloids on the shoulders can develop following injuries or surgeries in this region. They may pose challenges due to the potential for friction with clothing.
- Keloids on Jawline: Keloids on the jawline are often associated with acne scarring. These growths may be noticeable and impact the appearance of the face.
- Keloids on Ankles: Keloids on the ankles may result from injuries, surgical scars, or burns in this area. The lower extremities can be susceptible to keloid formation due to constant movement.
- Keloids on Back: Keloids on the back may arise from surgical scars, injuries, or burns. These growths may be challenging to manage due to their location.
- *Keloids on Arms:* Keloids on the arms can develop from various causes, including injuries, burns, or surgical scars. The arms, like other areas with frequent movement, may be prone to keloid formation.
Leukoderma

Leukoderma
Leukoderma: Unraveling Symptoms, Causes, and Types
Leukoderma, also known as vitiligo, is a skin disorder characterized by the development of depigmented patches on the skin. These patches result from the loss of melanocytes, the pigment-producing cells in the skin. Understanding the symptoms, causes, and types of leukoderma is essential for accurate diagnosis and effective management.
Symptoms:
- Depigmented Patches: The primary symptom of leukoderma is the presence of depigmented or white patches on the skin. These patches can vary in size and shape and may gradually enlarge over time.
- Symmetrical Distribution: In many cases, leukoderma exhibits a symmetrical distribution, meaning that depigmented patches appear on both sides of the body in corresponding locations.
- Common Sites: Leukoderma often affects areas exposed to the sun, such as the face, hands, arms, feet, and areas around body openings like the eyes and mouth.
- Hair and Color Changes: In addition to skin depigmentation, individuals with leukoderma may experience a loss of color in the hair located within the affected patches, turning them white or gray.
- Koebner Phenomenon: Some people with leukoderma may experience the Koebner phenomenon, where new depigmented patches develop at sites of skin trauma, such as cuts, scratches, or burns.
- Eyelash and Eyebrow Involvement: Leukoderma can also affect the eyelashes and eyebrows, leading to depigmentation in these areas.
- Mucous Membrane Involvement: In rare cases, leukoderma may extend to involve the mucous membranes, leading to depigmented patches inside the mouth or on the genitalia.
- No Other Symptoms: Leukoderma typically does not cause other physical symptoms, such as itching or pain, but the cosmetic impact can significantly affect an individual’s emotional well-being.
Causes:
- Autoimmune Factors: One of the leading theories behind leukoderma is an autoimmune response, where the body’s immune system mistakenly attacks and destroys its own melanocytes. Genetic factors may contribute to this autoimmune response.
- Genetic Predisposition: There is a genetic component to leukoderma, with a higher risk in individuals with a family history of the condition. Certain genes associated with the immune system and melanocyte function may play a role.
- Neural Theory: Some researchers propose the neural theory, suggesting that biochemical substances released from nerve endings may be toxic to melanocytes, leading to their destruction and the development of depigmented patches.
- Oxidative Stress: Oxidative stress, caused by an imbalance between free radicals and antioxidants in the body, has been implicated in the development of leukoderma. This oxidative stress may contribute to the destruction of melanocytes.
- Viral Infections: Certain viral infections, such as herpes simplex, have been linked to the onset or exacerbation of leukoderma in some individuals. The exact mechanisms are not fully understood.
- Environmental Triggers: Exposure to certain environmental factors, such as chemicals or industrial pollutants, may trigger leukoderma in susceptible individuals.
- Hormonal Changes: Changes in hormonal levels, particularly during puberty or pregnancy, may influence the development or progression of leukoderma.
- Neurochemical Factors: Imbalances in neurochemicals, including neuropeptides, have been proposed as potential contributors to leukoderma.
- Psychological Stress: While stress is not a direct cause, it can potentially exacerbate leukoderma in individuals who already have the condition.
Types:
- Non-Segmental Vitiligo: This is the most common type of leukoderma, characterized by depigmented patches that are widespread and often symmetrical. Non-segmental vitiligo can further be classified into focal, mucosal, acrofacial, and generalized subtypes.
– Focal Vitiligo: Involves one or a few isolated depigmented patches.
– Mucosal Vitiligo: Affects mucous membranes, leading to depigmentation inside the mouth or on the genitalia.
– Acrofacial Vitiligo: Predominantly involves the face, hands, and feet.
– Generalized Vitiligo: The most common subtype, with widespread depigmentation on various parts of the body.
- Segmental Vitiligo: This type is characterized by depigmented patches that are localized to one side or segment of the body. Segmental vitiligo usually develops at an earlier age than non-segmental vitiligo.
- Mixed Vitiligo: Some individuals may have features of both non-segmental and segmental vitiligo, leading to a diagnosis of mixed vitiligo.
Lichen Planus

Lichen Planus
Lichen Planus: Unraveling Symptoms, Causes, and Types
Lichen planus is a chronic inflammatory skin condition that can affect various parts of the body, mucous membranes, and nails. It is characterized by the development of flat-topped, itchy, and often polygonal-shaped papules or lesions. Understanding the symptoms, causes, and types of lichen planus is essential for proper diagnosis and management.
Symptoms:
- Skin Lesions: The hallmark symptom of lichen planus is the presence of skin lesions. These lesions are typically purplish, flat-topped bumps that may have a shiny surface. They can vary in size and shape, and when grouped, they often form a pattern resembling lace.
- Itching: Lichen planus is often accompanied by intense itching, which can range from mild to severe. The itching can significantly impact the affected individual’s quality of life.
- Nail Changes: In some cases, lichen planus can affect the nails, leading to changes such as ridges, grooves, or pitting. The nails may become thin or brittle.
- Oral Lesions: Lichen planus can involve the mucous membranes, particularly in the mouth. Oral lesions may present as white, lacy patches, ulcers, or red, swollen areas.
- Scalp Involvement: Lichen planus can affect the scalp, leading to redness, itching, and the development of lesions. Hair loss may occur in the affected areas.
- Genital Involvement: Genital lichen planus can cause lesions on the genital skin, leading to discomfort, pain, or itching.
- Hyperpigmentation or Hypopigmentation: As lichen planus lesions heal, they may leave behind areas of hyperpigmentation (darkened skin) or hypopigmentation (lightened skin).
- Koebner Phenomenon: Some individuals with lichen planus may experience the Koebner phenomenon, where new lesions develop at sites of skin trauma or injury.
Causes:
The exact cause of lichen planus is not well understood, but it is believed to involve an abnormal immune response. Potential triggers and factors associated with lichen planus include:
- Autoimmune Response: Lichen planus is thought to be an autoimmune condition where the body’s immune system mistakenly attacks its own cells, leading to inflammation and the development of lesions.
- Genetic Predisposition: There may be a genetic component, as lichen planus sometimes occurs in families. Certain genetic factors may contribute to an individual’s susceptibility to the condition.
- Viral Infections: Some viral infections, including hepatitis C, may be associated with the development or exacerbation of lichen planus in susceptible individuals.
- Stress: While not a direct cause, stress and emotional factors may play a role in triggering or exacerbating lichen planus in some individuals.
- Contact Allergens: Exposure to certain chemicals or allergens may contribute to the development of lichen planus, especially in the oral or genital areas.
- Dental Restorations: Dental materials, particularly dental amalgam, have been suggested as potential triggers for oral lichen planus in some individuals.
- Hormonal Factors: Hormonal changes, such as those occurring during menopause, may influence the development of lichen planus, especially in the genital area.
Types:
- Classic Lichen Planus: This is the most common form, characterized by the development of skin lesions on various parts of the body.
- Oral Lichen Planus: Involves the mucous membranes of the mouth and can present as white, lacy patches, red areas, or ulcers. It may cause discomfort or pain while eating or speaking.
- Genital Lichen Planus: Affects the genital area and can lead to lesions on the vulva, vagina, penis, or scrotum. It may cause itching, pain, or discomfort.
- Nail Lichen Planus: Involves the nails, leading to changes such as ridges, grooves, pitting, thinning, or brittleness.
- Scalp Lichen Planus: Affects the scalp and may cause redness, itching, and the development of lesions. Hair loss (scarring alopecia) may occur in severe cases.
- Linear Lichen Planus: Presents as lesions arranged in a linear or band-like pattern on the skin. This form may follow the lines of trauma or injury.
- Hypertrophic Lichen Planus: Characterized by thickened, raised lesions that may resemble keloids. This variant is less common but can be more resistant to treatment.
- Actinic Lichen Planus: Aggravated by sun exposure, this variant is more commonly seen in sun-exposed areas of the skin and may have hypertrophic features.
Lipoma

Lipoma
Lipoma: Unraveling Symptoms, Causes, and Types
A lipoma is a common, benign (non-cancerous) soft tissue tumor that develops from fat cells. These slow-growing lumps are usually situated just beneath the skin and are typically painless. Understanding the symptoms, causes, and types of lipoma is crucial for accurate diagnosis and appropriate management.
Symptoms:
- Soft, Moveable Mass: The primary symptom of a lipoma is the presence of a soft, rubbery lump beneath the skin. These lumps are typically painless and easily moveable when touched.
- 2. Slow Growth: Lipomas tend to grow slowly over time. While they are usually small, some lipomas can reach sizes of several inches in diameter.
- Color and Texture: Lipomas are generally colorless and have a doughy or rubbery texture. They are often found just beneath the skin’s surface.
- Painless: Lipomas are typically painless, although some individuals may experience discomfort if the lipoma presses on nerves or other structures.
- Location: Lipomas can occur anywhere on the body but are most commonly found on the shoulders, neck, chest, back, thighs, or arms.
- Rare Symptoms: In rare cases, lipomas may cause symptoms if they press on nearby nerves or blood vessels. This can result in pain, tenderness, or a feeling of fullness in the affected area.
Causes:
- Genetic Predisposition: There may be a genetic component to the development of lipomas, as they sometimes run in families. Certain genetic conditions, such as adiposis dolorosa, are associated with an increased risk of lipoma formation.
- Age: Lipomas are most commonly diagnosed in adults between the ages of 40 and 60. However, they can occur at any age.
- Inheritance: While most lipomas occur sporadically, some individuals may inherit a predisposition to developing these fatty tumors.
- Adipocyte Proliferation: Lipomas are believed to arise from an overgrowth of fat cells (adipocytes). The exact mechanism triggering this proliferation is not fully understood.
- Soft Tissue Injuries: Some studies suggest a potential link between soft tissue injuries and the development of lipomas, although more research is needed to establish a clear connection.
- Chromosomal Abnormalities: In cases of familial multiple lipomatosis, individuals may have specific chromosomal abnormalities that increase their susceptibility to lipoma development.
- Hormonal Factors: Hormonal imbalances or changes may contribute to the growth of lipomas in some cases, although the relationship is not well-defined.
- Trauma: While the role of trauma is debated, some believe that injuries or trauma to fatty tissue may trigger the formation of lipomas in susceptible individuals.
Types:
- Classic Lipoma: The most common type, these lipomas are typically small, soft, and slow-growing. They are found just beneath the skin and are usually painless.
- Superficial Subcutaneous Lipoma: Located just beneath the skin, these lipomas are easily felt and moved. They are the typical presentation of a lipoma.
- Deep Infiltrating Lipoma: These lipomas are situated deeper within the muscles and may be more challenging to diagnose. They can grow large and occasionally cause symptoms if they press on surrounding structures.
- Intramuscular Lipoma: Found within muscle tissue, these lipomas can sometimes cause pain or discomfort, especially if they compress nerves or blood vessels.
- Angiolipoma: This variant contains more blood vessels and may be more tender than the classic lipoma. Angiolipomas are also more likely to be painful.
- Hibernoma: A rare type of lipoma that contains brown fat, hibernomas are often found in areas rich in brown fat, such as the neck, shoulders, and back.
- Spindle Cell Lipoma: This variant has a more fibrous appearance due to the presence of spindle-shaped cells. It is typically found on the neck or shoulders and may be more common in men.
- Pleomorphic Lipoma: Occurring most frequently in elderly men, pleomorphic lipomas have a distinct appearance with multiple cell types. They are often found on the neck or upper back.
- Atypical Lipomatous Tumor (ALT) or Well-Differentiated Liposarcoma: Although considered a form of liposarcoma, ALT is a low-grade malignancy. It may appear similar to a benign lipoma but requires careful monitoring and surgical management.
Melasma

Melasma
Melasma: Unveiling Symptoms, Causes, and Types
Melasma is a common skin condition characterized by the development of brown or grayish-brown patches on the face, particularly on areas exposed to sunlight. While it is generally benign, melasma can have a significant impact on one’s appearance and self-esteem. Understanding the symptoms, causes, and types of melasma is essential for effective management and treatment.
Symptoms:
- Hyperpigmented Patches: The primary symptom of melasma is the presence of hyperpigmented patches on the skin. These patches are usually brown or grayish-brown and have well-defined borders.
- Location: Melasma typically occurs on sun-exposed areas of the face, such as the forehead, cheeks, nose, upper lip, and chin. It may also affect other sun-exposed areas like the neck and forearms.
- Symmetrical Distribution: Melasma often presents with a symmetrical distribution, meaning that the patches appear on both sides of the face in a similar pattern.
- Increased Pigmentation: The affected areas have increased pigmentation compared to the surrounding skin. The color of the patches can vary, and they may darken with sun exposure.
- Shape and Size: Melasma patches can vary in shape and size, ranging from small, round spots to larger, irregular patches.
- No Other Symptoms: Melasma does not cause other physical symptoms, such as itching, pain, or irritation. It is primarily a cosmetic concern.
- Exacerbation with Sun Exposure: Sun exposure is a significant factor that can worsen melasma. The condition may improve in the winter or when individuals avoid prolonged sun exposure.
Causes:
- Hormonal Factors: Hormonal changes are a major contributing factor to melasma. It is commonly associated with pregnancy (chloasma or “mask of pregnancy”) due to increased hormone levels. Hormonal contraception and hormone replacement therapy can also trigger melasma.
- Sun Exposure: Ultraviolet (UV) radiation from the sun is a key factor in the development of melasma. Sun exposure stimulates the production of melanin, the pigment responsible for skin color, leading to increased pigmentation in affected areas.
- Genetic Predisposition: There appears to be a genetic predisposition to melasma, as it often occurs in families. Individuals with a family history of melasma may be more prone to developing the condition.
- Ethnicity: Melasma is more prevalent in individuals with darker skin types, including those of Hispanic, Asian, Middle Eastern, and African descent.
- Cosmetic Products: Certain cosmetic products, especially those that irritate the skin, can contribute to melasma. This is known as post-inflammatory hyperpigmentation.
- Thyroid Dysfunction: Some cases of melasma have been associated with thyroid dysfunction, particularly when thyroid hormones are elevated.
- Medications: Certain medications, such as oral contraceptives, hormone replacement therapy, and antiepileptic drugs, may increase the risk of melasma.
- Cosmetic Procedures: Laser treatments, chemical peels, and other cosmetic procedures that cause skin irritation or inflammation can trigger melasma in susceptible individuals.
- Stress: While the relationship is not fully understood, stress has been suggested as a potential factor in the development or exacerbation of melasma.
Types:
- Epidermal Melasma: This type involves increased pigmentation in the epidermis, the outermost layer of the skin. The pigmentation is brown and well-defined.
- Dermal Melasma: In dermal melasma, pigmentation extends into the dermis, the deeper layer of the skin. The patches are grayish-brown and less well-defined.
- Mixed Melasma: Mixed melasma involves a combination of both epidermal and dermal components. It is the most common type and often presents with brown to grayish-brown patches.
- Extracutaneous Melasma: In rare cases, melasma may affect areas other than the skin, such as the oral mucosa (oral melasma) or the conjunctiva (ocular melasma).
Meniere’s disease

Meniere’s disease
Meniere’s Disease Overview:
Meniere’s disease is a disorder of the inner ear that causes episodes of vertigo, fluctuating hearing loss, tinnitus (ringing in the ear), and a feeling of fullness or pressure in the ear. It typically affects only one ear and can lead to significant disruption in daily life.
Symptoms:
- Vertigo: Episodes of severe dizziness or spinning sensations, often accompanied by nausea and vomiting.
- Hearing Loss: Fluctuating hearing loss, which may become permanent over time.
- Tinnitus: Ringing, buzzing, or roaring sounds in the affected ear.
- Aural Fullness: Feeling of pressure or fullness in the ear, similar to the sensation experienced during airplane takeoff or landing.
Causes:
The exact cause of Meniere’s disease is unknown, but it’s believed to be related to fluid buildup in the inner ear. Factors such as abnormal immune response, genetics, viral infections, and allergies may contribute to its development.
Diagnosis:
Diagnosing Meniere’s disease involves a combination of medical history, physical examination, and hearing tests (audiometry). Additional tests such as vestibular function tests, MRI, and blood tests may be conducted to rule out other potential causes.
Treatment:
- Medications: Prescribed medications such as diuretics, anti-nausea drugs, and vestibular suppressants may help alleviate symptoms.
- Lifestyle Changes: Dietary modifications (reducing salt intake), stress management techniques, and avoiding triggers (such as caffeine and alcohol) can help manage symptoms.
- Therapies: Physical therapy, vestibular rehabilitation therapy, and cognitive behavioral therapy may be recommended to improve balance and coping strategies.
- Surgical Options: In severe cases, surgical procedures such as endolymphatic sac decompression, vestibular nerve section, or inner ear injections may be considered.
Prognosis:
The course of Meniere’s disease varies from person to person. Some individuals may experience spontaneous remission of symptoms, while others may have persistent or progressive symptoms that significantly impact their quality of life. With proper management and treatment, many people can effectively manage their symptoms and lead fulfilling lives.
Molluscumcontagiosum

Molluscumcontagiosum
Molluscum Contagiosum: Unraveling Symptoms, Causes, and Types
Molluscum contagiosum is a viral skin infection that primarily affects children but can occur in individuals of any age. This condition is characterized by the appearance of small, raised, and painless bumps on the skin. Understanding the symptoms, causes, and types of molluscum contagiosum is essential for proper diagnosis and management.
Symptoms:
- Bumps or Lesions: The primary and most characteristic symptom of molluscum contagiosum is the development of small, dome-shaped bumps or lesions on the skin. These bumps are typically pearly or flesh-colored and have a central indentation or dimple.
- Size and Number: The size of the bumps can vary, but they are generally small, ranging from 2 to 5 millimeters in diameter. Clusters of bumps may appear, and the number of lesions can range from just a few to several dozen.
- Central Dimple: Each bump often has a central dimple or umbilication, which gives them a distinctive appearance. This central dimple is a key feature that helps distinguish molluscum contagiosum from other skin conditions.
- Itching: In some cases, the affected areas may become itchy. Scratching the lesions can lead to the spread of the virus to adjacent skin areas.
- Inflammation: The surrounding skin may become red and inflamed due to the body’s immune response to the viral infection.
- Location: Molluscum contagiosum lesions commonly appear on the face, neck, arms, hands, and other areas of the body. In adults, genital areas may also be affected.
- Painless: The lesions are typically painless, although itching or discomfort may occur, especially as the immune system responds to the infection.
Causes:
- Viral Infection: Molluscum contagiosum is caused by the molluscum contagiosum virus (MCV), a poxvirus. There are four distinct types of MCV (MCV-1 to MCV-4), with MCV-1 being the most common cause of infections in humans.
- Direct Skin-to-Skin Contact: The primary mode of transmission is through direct skin-to-skin contact. The virus can also be spread indirectly through fomites (inanimate objects that carry the virus, such as towels or toys).
- Children and Adolescents: Molluscum contagiosum is more common in children and adolescents, likely due to the increased likelihood of close contact in these age groups.
- Sexual Transmission: In adults, molluscum contagiosum can be sexually transmitted, especially in cases involving lesions in the genital or pubic areas. It is considered a sexually transmitted infection (STI) in these instances.
- Weakened Immune System: Individuals with weakened immune systems, such as those with HIV/AIDS or undergoing immunosuppressive treatments, may be more susceptible to molluscum contagiosum and may experience more prolonged or severe infections.
Types:
- Localized Molluscum Contagiosum:
– Characteristics: This is the most common type, characterized by a small number of lesions, typically less than 20.
– Location: Lesions are often localized to one area of the body.
- Generalized Molluscum Contagiosum:
– Characteristics: In this type, a larger number of lesions are present, often exceeding 20.
– Location: Lesions can appear on multiple areas of the body, leading to a more widespread distribution.
- Molluscum Contagiosum Eczematous Dermatitis:
– Characteristics: This variant is associated with eczematous dermatitis, where the lesions are surrounded by inflamed and itchy skin.
– Location: The inflammatory response may lead to more significant discomfort.
- Giant Molluscum Contagiosum:
– Characteristics: This rare form involves larger lesions that can be several centimeters in diameter.
– Location: The size of the lesions sets this variant apart from typical molluscum contagiosum.
- Molluscum Contagiosum with Immune Suppression:
– Characteristics: Individuals with compromised immune systems, such as those with HIV/AIDS, may experience a more severe and prolonged course of molluscum contagiosum.
Nail disorders

Nail disorders
Nail Disorders: Unveiling Symptoms, Causes, and Types
Nail disorders encompass a range of conditions affecting the nails, which can include changes in color, texture, thickness, or shape. These disorders can result from various factors, including infections, underlying health conditions, trauma, or genetic predispositions. Understanding the symptoms, causes, and types of nail disorders is vital for accurate diagnosis and appropriate management.
Symptoms:
- Changes in Color: Discoloration of the nails is a common symptom of nail disorders. Nails may appear yellow, brown, green, or even have white spots or streaks.
- Changes in Thickness: Abnormal thickening or thinning of the nails can occur. Thickened nails may be difficult to trim, while thin nails may be more prone to breakage.
- Changes in Texture: Alterations in the texture of the nails can manifest as ridges, pitting, grooves, or brittleness. Smooth, even texture is characteristic of healthy nails.
- Changes in Shape: Abnormalities in nail shape, such as clubbing (enlargement and rounding of fingertips), spooning (concave shape), or pincer nails, may indicate an underlying disorder.
- Pain or Discomfort: Some nail disorders can cause pain or discomfort, especially if there is an infection, ingrown nail, or injury.
- Separation from Nail Bed: Onycholysis refers to the separation of the nail from the underlying nail bed. This can result in a gap between the nail and the flesh.
- Swelling and Inflammation: Inflammatory conditions may cause swelling around the nails, redness, and tenderness.
- Brittle or Crumbly Nails: Nails that are excessively brittle or crumbly may indicate nutritional deficiencies, fungal infections, or other underlying issues.
Causes:
- Fungal Infections: Fungal infections, particularly onychomycosis, are a common cause of nail disorders. Fungi thrive in warm, moist environments, making nails susceptible to infection.
- Bacterial Infections: Bacterial infections, such as paronychia, can lead to redness, swelling, and pus around the nail.
- Viral Infections: Viruses like the human papillomavirus (HPV) can cause warts around or under the nails.
- Trauma: Physical trauma to the nails, such as crushing, slamming, or repetitive stress, can lead to various nail disorders, including subungual hematoma or traumatic nail dystrophy.
- Psoriasis: Psoriasis, an autoimmune condition, can affect the nails, causing pitting, ridges, and discoloration.
- Eczema (Dermatitis): Eczema or dermatitis can lead to redness, itching, and inflammation around the nails.
- Lichen Planus: Lichen planus is an inflammatory condition that can affect the nails, leading to ridges, grooves, and discoloration.
- Nutritional Deficiencies: Inadequate intake of essential nutrients like biotin, iron, or zinc can contribute to nail disorders.
- Systemic Diseases: Conditions such as diabetes, thyroid disorders, and autoimmune diseases can manifest with nail abnormalities.
- Medications: Certain medications, including chemotherapy drugs, antibiotics, and antifungal medications, can affect nail health.
- Allergies: Allergic reactions to nail products, such as nail polish or acrylic nails, can lead to nail disorders.
Types:
- Onychomycosis (Fungal Nail Infection):
– Symptoms: Thickened, discolored nails with possible brittleness.
– Causes: Fungal infections by dermatophytes, yeast, or molds.
– Treatment: Antifungal medications, topical or oral, are commonly used.
- Paronychia (Bacterial Infection):
– Symptoms: Redness, swelling, and pus around the nail.
– Causes: Bacterial infection, often due to injury, nail biting, or exposure to irritants.
– Treatment: Warm soaks, antibiotics for bacterial infections.
- Ingrown Toenail (Onychocryptosis):
– Symptoms: Pain, redness, and swelling along the nail edge.
– Causes: Nails growing into the surrounding skin, often due to improper trimming or tight shoes.
– Treatment: Warm soaks, proper nail trimming, antibiotics for infections, or surgical intervention in severe cases.
- Psoriatic Nails (Psoriasis):
– Symptoms: Pitting, ridges, discoloration, and separation from the nail bed.
– Causes: Psoriasis, an autoimmune condition affecting the skin and nails.
– Treatment: Topical or systemic medications to manage psoriasis.
- Lichen Planus Nails:
– Symptoms: Ridging, grooving, and nail thinning.
– Causes: Lichen planus, an inflammatory skin condition.
– Treatment: Topical or systemic steroids, depending on the severity.
- Onychogryphosis (Ram’s Horn Nails):
– Symptoms: Overgrowth of the nails, leading to a curved or horn-like appearance.
– Causes: Often associated with neglect, trauma, or underlying health conditions.
– Treatment: Regular trimming, management of underlying causes.
- Yellow Nail Syndrome:
– Symptoms: Yellow discoloration, thickening, and slow growth of nails.
– Causes: Respiratory or lymphatic conditions leading to poor nail growth.
– Treatment: Addressing underlying health conditions, nutritional support.
- Beau’s Lines:
– Symptoms: Transverse depressions or ridges across the nails.
– Causes: Interrupted nail growth due to severe illness, trauma, or systemic conditions.
– Treatment: Managing underlying causes, as Beau’s lines grow out with time.
- Koilonychia (Spoon Nails):
– Symptoms: Concave or spoon-shaped nails.
– Causes: Iron deficiency anemia, hemochromatosis, or certain genetic conditions.
– Treatment: Addressing underlying causes, iron supplementation if needed.
Neurodermatitis

Neurodermatitis
Neurodermatitis: Understanding Symptoms, Causes, and Types
Neurodermatitis, also known as lichen simplex chronicus, is a skin condition characterized by chronic itching and scratching that leads to thickened, leathery patches of skin. This condition is often linked to psychological or emotional factors and can significantly impact a person’s quality of life. To grasp the intricacies of neurodermatitis, it’s essential to explore its symptoms, causes, and various types.
Symptoms:
The hallmark symptom of neurodermatitis is persistent itching, typically in a localized area. As individuals scratch or rub the affected area repeatedly, several symptoms may develop:
- Itchy Skin: The primary symptom is intense itching, which can become a persistent and overwhelming sensation.
- Thickened Skin: Continuous scratching and rubbing lead to thickened, leathery patches of skin, especially in the affected area.
- Redness: The skin may appear red or inflamed due to chronic irritation.
- Raised Lesions: Prolonged scratching can result in raised, scaly, or lichenified lesions.
- Hyperpigmentation: Darkening of the skin may occur in chronic cases, particularly in individuals with darker skin tones.
- Bleeding: Excessive scratching can cause small cuts or abrasions, leading to bleeding.
Causes:
The exact cause of neurodermatitis is multifaceted and often involves a combination of factors. Common contributors include:
- Itching and Scratching Response: Neurodermatitis often begins with an initial skin irritation or itch, which prompts the individual to scratch. However, the repeated scratching creates a cycle where the skin becomes more irritated, leading to further itching and scratching.
- Psychological Factors: Stress, anxiety, or emotional distress are frequently associated with the development or exacerbation of neurodermatitis. Psychological factors can contribute to increased sensitivity to itching.
- Skin Irritants: Exposure to irritants, such as harsh soaps, detergents, or certain fabrics, can trigger or worsen neurodermatitis.
- Underlying Skin Conditions: Pre-existing skin conditions like eczema or psoriasis can increase the risk of developing neurodermatitis.
- Nerve Dysfunction: Some researchers suggest that dysfunction in nerve signaling may play a role in neurodermatitis, contributing to heightened sensitivity to itching.
- Genetic Predisposition: A family history of atopic dermatitis or other skin disorders may increase the likelihood of developing neurodermatitis.
Types:
- Localized Neurodermatitis:
– Symptoms: Itching and thickened skin patches are confined to a specific area, often on the back of the neck, scalp, ankles, wrists, or genital region.
– Causes: Localized irritants, psychological stress, or a history of skin conditions can contribute to this type.
- Generalized Neurodermatitis:
– Symptoms: Itching and thickened skin patches occur more widespread across the body.
– Causes: Psychological factors, stress, or systemic conditions may contribute to generalized neurodermatitis.
- Pompholyx Neurodermatitis (Dyshidrotic Eczema):
– Symptoms: Itchy blisters, often on the hands and feet, accompanied by redness and peeling.
– Causes: Irritants, stress, or a predisposition to eczema may contribute.
- Linear Neurodermatitis:
– Symptoms: Itching and thickened skin patches occur in a linear or band-like pattern.
– Causes: Physical trauma or repetitive scratching along a specific path may lead to linear neurodermatitis.
Non-healing ulcers

Non-healing ulcers
Non-Healing Ulcers: Understanding Symptoms, Causes, and Types
Non-healing ulcers are chronic wounds that fail to progress through the normal phases of healing within an expected timeframe. These ulcers can be persistent, leading to complications and posing challenges in their management. Key aspects of non-healing ulcers, including symptoms, causes, and types, are essential to address for effective treatment.
Symptoms:
The hallmark symptom of non-healing ulcers is the persistence of an open wound without signs of improvement. Other common symptoms include:
- Prolonged Wound Presence: The primary indicator is the continued existence of the ulcer without significant healing progress.
- Pain or Discomfort: Non-healing ulcers can be associated with pain or discomfort, which may vary in intensity.
- Inflammation: Redness and swelling around the ulcer site may indicate ongoing inflammation, potentially caused by infection or impaired healing.
- Odor: In some cases, non-healing ulcers may produce an unpleasant odor, often associated with infection or necrotic tissue.
Causes:
Several factors contribute to the development of non-healing ulcers, and the underlying cause can vary. Common causes include:
- Poor Blood Circulation: Inadequate blood flow to the affected area, often due to conditions like peripheral artery disease, can impede the healing process.
- Diabetes: Individuals with diabetes are prone to develop ulcers, particularly on the feet, due to nerve damage and poor circulation.
- Infection: Bacterial, fungal, or viral infections can hinder wound healing, leading to chronic ulcers.
- Pressure Ulcers: Prolonged pressure on a specific area, commonly seen in bedridden individuals, can result in non-healing ulcers known as pressure ulcers or bedsores.
- Autoimmune Disorders: Conditions like vasculitis or lupus can cause inflammation in blood vessels, affecting proper wound healing.
- Malnutrition: Inadequate nutrition can compromise the body’s ability to repair and regenerate tissues, contributing to non-healing ulcers.
- Underlying Health Conditions: Chronic illnesses such as HIV, certain cancers, or autoimmune disorders may impede the healing process.
- Venous Insufficiency: Poor functioning of the venous valves can lead to chronic venous ulcers, often seen in the lower legs.
Types:
- Arterial Ulcers:
– Causes: Insufficient blood flow due to arterial disease, atherosclerosis, or peripheral artery disease.
– Location: Commonly found on the lower extremities, especially toes or heels.
– Characteristics: Painful, with well-defined edges and minimal exudate.
- Venous Ulcers:
– Causes: Poor venous circulation, often associated with chronic venous insufficiency.
– Location: Typically on the lower legs, near the ankles.
– Characteristics: Edges are irregular, and ulcers may have moderate to high exudate.
- Pressure Ulcers (Bedsores):
– Causes: Prolonged pressure on specific areas, commonly in bedridden or immobile individuals.
– Location: Bony prominences like the hips, heels, or sacrum.
– Characteristics: Varying stages of severity, from superficial to deep wounds.
- Diabetic Ulcers:
– Causes: Neuropathy, poor circulation, and impaired immune function in individuals with diabetes.
– Location: Often on the feet, especially pressure points.
– Characteristics: May be painless initially, with potential for infection.
- Neuropathic Ulcers:
– Causes: Nerve damage, often associated with conditions like diabetes.
– Location: Areas subjected to repetitive trauma or pressure.
– Characteristics: Lack of pain due to nerve damage, may have irregular edges.
Addressing the underlying cause is crucial for the effective treatment of non-healing ulcers. A comprehensive approach involving wound care, infection management, and addressing contributing factors such as circulation or nutritional issues is essential for successful ulcer healing. Early intervention and a multidisciplinary approach with healthcare professionals are key in managing non-healing ulcers.
Pemphigus Vulgaris

Pemphigus Vulgaris
Pemphigus Vulgaris: Unraveling Symptoms, Causes, and Types
Pemphigus vulgaris is a rare autoimmune disorder characterized by the formation of painful blisters and erosions on the skin and mucous membranes. This condition occurs when the immune system mistakenly targets proteins that play a crucial role in maintaining the structure of skin cells. Understanding the symptoms, causes, and types of pemphigus vulgaris is essential for diagnosis and appropriate management.
Symptoms of Pemphigus Vulgaris:
- Blisters:
– The hallmark symptom is the development of fragile, fluid-filled blisters on the skin and mucous membranes. These blisters are prone to rupture, leaving painful, open sores.
- Oral Lesions:
– Blisters often occur in the mouth, leading to painful oral erosions. This can make eating and speaking difficult.
- Skin Erosions:
– As blisters rupture, they give rise to raw and painful erosions on the skin, which can be widespread.
- Pain and Itching:
– Affected individuals often experience pain, burning, and itching associated with the blisters and erosions.
- Nail Involvement:
– In some cases, pemphigus vulgaris can affect the nails, leading to changes such as nail loss or deformities.
- Ocular Involvement:
– In rare instances, the eyes may be affected, causing irritation, redness, and sensitivity to light.
- General Malaise:
– The condition can be associated with a general feeling of unwellness, fatigue, and weight loss.
Causes of Pemphigus Vulgaris:
Pemphigus vulgaris is an autoimmune disorder, meaning that the immune system mistakenly attacks healthy cells. The specific cause of this immune system malfunction is not fully understood, but it is believed to involve the production of antibodies targeting proteins called desmogleins, which are essential for maintaining the structure and adhesion of skin cells.
Types of Pemphigus Vulgaris:
- Pemphigus Vulgaris:
– The most common form of pemphigus, characterized by the development of blisters and erosions on the skin and mucous membranes.
- Pemphigus Foliaceus:
– Similar to pemphigus vulgaris, but the blisters in pemphigus foliaceus are usually confined to the upper layers of the skin, causing scaly and crusted lesions. It tends to spare mucous membranes.
- Paraneoplastic Pemphigus:
– A rare and severe form of pemphigus associated with underlying malignancies, such as lymphomas. It often involves the mucous membranes and can lead to severe complications.
- IgA Pemphigus:
– Characterized by the presence of IgA antibodies rather than IgG antibodies. It can present with vesicles, pustules, or bullae on the skin.
- Drug-Induced Pemphigus:
– Certain medications, particularly those used in treating high blood pressure and rheumatoid arthritis, can induce pemphigus-like symptoms.
Pityriasis Alba

Pityriasis Alba
Pityriasis Alba: Unraveling Symptoms, Causes, and Types
Pityriasis alba is a common skin condition that primarily affects children and adolescents. It is characterized by the presence of round or oval, pale patches on the skin, often on the face. Understanding the symptoms, causes, and types of pityriasis alba is essential for proper diagnosis and management.
Symptoms of Pityriasis Alba:
- Hypopigmented Patches:
– The hallmark symptom of pityriasis alba is the development of light-colored or hypopigmented patches on the skin. These patches are usually round or oval and may vary in size.
- Dry and Scaly Skin:
– The affected skin may appear dry and slightly scaly. However, it is not typically associated with significant itching or discomfort.
- Mild Redness:
– The patches may have a mild redness at the borders, creating a subtle contrast with the surrounding normal skin.
- Facial Involvement:
– Pityriasis alba commonly occurs on the face, particularly on the cheeks. However, it can also affect other areas of the body, such as the arms or trunk.
- Exacerbation with Sun Exposure:
– The patches may become more noticeable after sun exposure due to the contrast between the affected and unaffected skin.
- Resolution without Scarring:
– Pityriasis alba tends to resolve on its own over time, and it does not leave scarring on the skin.
Causes of Pityriasis Alba:
- Atopic Dermatitis (Eczema):
– There is a strong association between pityriasis alba and atopic dermatitis, a chronic skin condition characterized by inflammation and itching. Pityriasis alba patches may develop as a post-inflammatory response.
- Genetic Factors:
– Genetic predisposition may play a role in the development of pityriasis alba. Individuals with a family history of atopic conditions like eczema may be more prone to this skin condition.
- Dry Skin:
– Pityriasis alba is more common in individuals with dry skin. Lack of moisture can contribute to the development of the characteristic hypopigmented patches.
- Sun Exposure:
– Sun exposure can exacerbate the appearance of pityriasis alba patches. The contrast between the affected and unaffected skin becomes more noticeable after sun exposure.
- Environmental Factors:
– Factors such as low humidity and harsh weather conditions can contribute to dry skin and may be linked to the development of pityriasis alba.
- Immunological Factors:
– Some research suggests that immune system dysregulation may contribute to the development of pityriasis alba, especially in individuals with atopic conditions.
Types of Pityriasis Alba:
- Classic Pityriasis Alba:
– This is the most common type, characterized by round or oval, hypopigmented patches on the face, particularly the cheeks. It is often associated with a history of atopic dermatitis.
- Facial Pityriasis Alba:
– When the condition primarily affects the face, it is referred to as facial pityriasis alba. The patches are usually symmetrical and may have a mild redness at the borders.
- Pityriasis Alba on Other Body Parts:
– Pityriasis alba can also occur on other body parts, such as the arms, trunk, or neck. The patches have similar characteristics of hypopigmentation and mild scaling.
Pityriasis Rosea

Pityriasis Rosea
Pityriasis Rosea: Unraveling Symptoms, Causes, and Types
Pityriasis rosea is a common skin condition characterized by the development of a distinctive rash. While the exact cause remains unclear, it is believed to be associated with viral infections. Understanding the symptoms, causes, and types of pityriasis rosea is essential for accurate diagnosis and appropriate management.
Symptoms of Pityriasis Rosea:
- Herald Patch:
– The initial symptom of pityriasis rosea is often a single, larger lesion called the “herald patch.” This patch is typically round or oval, with a pink or red border and a central area that may be lighter in color.
- Secondary Rash:
– Following the appearance of the herald patch, a secondary rash develops. This rash consists of smaller, similar-looking patches that may be scattered across the torso, arms, and legs. The distribution often creates a pattern resembling the branches of a tree.
- Itching:
– Itching is a common symptom, especially as the rash spreads. However, the degree of itching varies among individuals.
- Scaling:
– The patches may become slightly scaly, with fine scales on the surface. This is more noticeable as the rash progresses.
- Fever and Malaise:
– Some individuals may experience mild systemic symptoms such as low-grade fever, fatigue, or a general feeling of unwellness.
- Darkening of Skin:
– After the rash resolves, the affected skin may temporarily darken before returning to its normal color.
Causes of Pityriasis Rosea:
- Viral Infections:
– Pityriasis rosea is believed to be triggered by viral infections, with human herpesvirus (HHV) types 6 and 7 being commonly associated. The exact mechanism by which the virus leads to the development of the rash is not fully understood.
- Seasonal Variation:
– There may be a seasonal variation in the incidence of pityriasis rosea, with higher rates reported in the spring and fall. This seasonal pattern suggests a possible role of environmental factors or certain viral infections.
- Immunological Factors:
– Some researchers propose that immune responses to viral infections may play a role in the development of pityriasis rosea. The condition is not considered contagious, and direct person-to-person transmission is uncommon.
- Genetic Factors:
– There may be a genetic predisposition to pityriasis rosea, as it is more commonly reported in individuals with a family history of the condition.
Types of Pityriasis Rosea:
- Classic Pityriasis Rosea:
– The classic form of pityriasis rosea follows the typical course, starting with the appearance of the herald patch, followed by the development of smaller patches in a distinct pattern.
- Inverse Pityriasis Rosea:
– In this variant, the rash develops in areas where skin surfaces touch or rub against each other, such as the armpits, groin, or under the breasts. The distribution may deviate from the typical pattern.
- Giant Pityriasis Rosea:
– Giant pityriasis rosea is characterized by larger and more widespread lesions than the classic form. The patches may be more extensive and take longer to resolve.
- Hemorrhagic Pityriasis Rosea:
– This rare subtype is characterized by the presence of hemorrhagic lesions, where the patches exhibit bleeding or purpura. It is considered an atypical presentation.
- Papular Pityriasis Rosea:
– Papular pityriasis rosea is distinguished by the presence of small papules or raised bumps within the rash, giving it a different appearance from the typical flat lesions.
Pityriasis Versicolor

Pityriasis Versicolor
Pityriasis Versicolor: Decoding Symptoms, Causes, and Types
Pityriasis versicolor, also known as tinea versicolor, is a common skin condition caused by an overgrowth of a yeast-like fungus. This condition often presents with characteristic skin discoloration and can vary in appearance. Understanding the symptoms, causes, and types of pityriasis versicolor is crucial for accurate diagnosis and effective treatment.
Symptoms of Pityriasis Versicolor:
- Hypo – or Hyperpigmented Patches:
– The hallmark of pityriasis versicolor is the development of discolored patches on the skin. These patches can be lighter (hypopigmented) or darker (hyperpigmented) than the surrounding skin.
- Scaling and Mild Itching:
– Affected areas may exhibit fine scaling, and some individuals may experience mild itching. The scaling is often more noticeable when the skin is scraped or scratched.
- Patchy Distribution:
– Patches can occur on various parts of the body, commonly on the trunk, shoulders, and upper arms. The distribution can be patchy, and the appearance may vary.
- Worsening in Sunlight:
– The contrast between the affected and unaffected skin may be more noticeable after sun exposure. This is because the yeast responsible for pityriasis versicolor, known as Malassezia, produces substances that interfere with pigmentation.
- Patches May Blend or Extend:
– Over time, the patches may blend or extend, creating larger areas of discoloration. The edges of the patches can be irregular, and the overall appearance may change.
- No Scarring:
– Pityriasis versicolor does not leave scars on the skin. However, the discoloration may persist even after the yeast is treated.
Causes of Pityriasis Versicolor:
- Malassezia Yeast Overgrowth:
– The primary causative agent for pityriasis versicolor is the Malassezia yeast, particularly Malassezia globosa and Malassezia furfur. These yeasts are naturally present on the skin, but overgrowth can lead to the development of the condition.
- Warm and Humid Environments:
– Malassezia yeasts thrive in warm and humid conditions. Pityriasis versicolor is more common in regions with such climates.
- Oily Skin:
– The yeast feeds on the oils produced by the skin. Individuals with naturally oily skin may be more susceptible to the overgrowth of Malassezia.
- Weakened Immune System:
– Conditions that weaken the immune system, such as HIV/AIDS or immunosuppressive medications, can increase the risk of developing pityriasis versicolor.
- Hormonal Changes:
– Hormonal changes, especially during adolescence, pregnancy, or while using hormonal contraceptives, may influence the development of the condition.
Types of Pityriasis Versicolor:
- Hypopigmented Pityriasis Versicolor:
– This type is characterized by lighter patches on the skin, which may be more noticeable in individuals with darker skin tones. The contrast between the affected and unaffected skin can be striking.
- Hyperpigmented Pityriasis Versicolor:
– In hyperpigmented pityriasis versicolor, the patches appear darker than the surrounding skin. This type is more common in individuals with lighter skin tones.
- Pityriasis Versicolor on the Face:
– While the trunk is the most commonly affected area, pityriasis versicolor can also occur on the face. Facial involvement may present with discoloration and mild scaling.
- Extensive or Generalized Pityriasis Versicolor:
– Some individuals may develop extensive or generalized involvement, where large areas of the body are affected. This can lead to a more widespread and pronounced appearance.
Pityriasis Corporis

Pityriasis Corporis
Pityriasis Corporis: Unveiling Symptoms, Causes, and Types
Pityriasis corporis, commonly known as tinea corporis or ringworm, is a fungal infection of the skin that typically presents as circular or ring-shaped rashes. Understanding the symptoms, causes, and types of pityriasis corporis is essential for proper diagnosis and effective treatment.
Symptoms of Pityriasis Corporis:
- Ring-Shaped Rash:
– The most characteristic symptom of pityriasis corporis is the presence of circular or ring-shaped rashes on the skin. These lesions often have a raised, red border with a clearer or more normal-looking center.
- Itching:
– Affected individuals commonly experience itching in and around the ring-shaped rashes. The intensity of itching can vary from mild to severe.
- Scaling and Flaking:
– The skin within the ring-shaped rash may become scaly and flaky. This is particularly noticeable as the infection progresses.
- Multiple Lesions:
– Pityriasis corporis can lead to the development of multiple lesions on different areas of the body. These lesions may vary in size and appearance.
- Clearing in the Center:
– The central area of the ring-shaped rash often clears, giving it a distinct appearance. This clearing is more pronounced as the infection resolves.
- Spread to Other Body Parts:
– The infection can spread to other body parts through direct contact with the affected skin or contaminated objects.
Causes of Pityriasis Corporis:
- Fungal Infection:
– Pityriasis corporis is caused by dermatophyte fungi, typically belonging to the genera Trichophyton or Microsporum. These fungi thrive on the keratin in the outer layer of the skin.
- Direct Contact:
– The fungus responsible for pityriasis corporis is often transmitted through direct skin-to-skin contact with an infected person or through contact with contaminated surfaces, such as towels or clothing.
- Animal Contact:
– Some forms of tinea corporis can be transmitted from animals to humans, such as from infected pets. This is more common with certain species, like cats or dogs.
- Warm and Humid Environments:
– Fungi that cause pityriasis corporis thrive in warm and humid environments. Sweating and inadequate ventilation can create favorable conditions for the infection to develop.
- Weakened Immune System:
– Individuals with weakened immune systems, such as those with HIV/AIDS or certain medical conditions, may be more susceptible to fungal infections, including pityriasis corporis.
- Shared Personal Items:
– Sharing personal items like combs, brushes, or clothing with an infected person can contribute to the transmission of the fungus.
Types of Pityriasis Corporis:
- Tinea Corporis Glabrous:
– This type primarily affects the glabrous (hairless) skin on various parts of the body. It is characterized by well-defined, red, scaly patches.
- Tinea Corporis Barbae:
– Tinea corporis barbae specifically affects the bearded areas of the face and neck. It can lead to the development of itchy, red, and scaly patches within the beard.
- Tinea Corporis Faciei:
– Tinea corporis faciei involves the face and typically affects the smooth skin, causing circular rashes with red borders and central clearing.
- Tinea Corporis Profunda:
– This less common type penetrates deeper into the skin layers, often resulting in more severe symptoms. It may require systemic antifungal medications for treatment.
Jock Itch

Jock Itch
Jock Itch: Unraveling Symptoms, Causes, and Types
Jock itch, medically known as tinea cruris, is a common fungal infection affecting the skin of the groin area. It belongs to a group of fungal skin infections called dermatophytosis. Understanding the symptoms, causes, and types of jock itch is essential for effective management and prevention of this bothersome condition.
Symptoms:
- Itching: The hallmark symptom of jock itch is itching in the groin area. The itching can range from mild to intense and is often accompanied by a persistent urge to scratch.
- Redness: The affected skin typically becomes red, creating a distinct border between the affected area and the surrounding skin.
- Rash: Jock itch manifests as a rash, which may have a raised edge and can extend to the inner thighs or buttocks. The rash often takes on a circular or oval shape.
- Burning Sensation: Some individuals may experience a burning sensation in the affected area, especially during physical activity or when the skin is moist.
- Flaking or Peeling: The skin affected by jock itch may start to flake or peel, contributing to the overall discomfort.
- Cracks or Blisters: In severe cases, jock itch may lead to the development of small cracks or blisters in the affected area.
- Pain: While jock itch is primarily characterized by itching, the persistent scratching and irritation can lead to pain in the affected region.
Causes:
- Fungal Infection: Jock itch is primarily caused by a type of fungus called dermatophytes. These fungi thrive in warm, moist environments, making the groin area an ideal location for their growth.
- Warm and Humid Conditions: Activities that result in increased sweating, combined with tight or non-breathable clothing, create an environment conducive to the growth of fungi. This is why jock itch is more common in individuals who engage in sports or have jobs that involve prolonged periods of physical activity.
- Sharing Contaminated Items: Sharing towels, clothing, or personal items with someone who has a fungal infection can increase the risk of acquiring jock itch.
- Weakened Immune System: Individuals with weakened immune systems, due to conditions such as diabetes or HIV, are more susceptible to fungal infections, including jock itch.
- Obesity: Excess weight can contribute to skin folds and increased sweating, creating an environment favorable for the development of jock itch.
- Tight Clothing: Wearing tight underwear or athletic supporters can trap moisture and heat, promoting fungal growth. This is particularly common in individuals who wear these items for extended periods.
Types:
- Classic Jock Itch: This is the typical form of jock itch characterized by redness, itching, and a rash in the groin area. It often occurs in individuals who engage in sports or activities that result in increased sweating.
- Inverse Jock Itch: Inverse jock itch affects the skin in the folds of the groin, buttocks, or inner thighs. It is more common in individuals who are overweight or those with deep skin folds.
- Chronic Jock Itch: Some individuals may experience persistent or recurrent episodes of jock itch, leading to chronic symptoms. This may be due to factors such as repeated exposure, incomplete treatment, or underlying health conditions.
- Secondary Bacterial Infection: In some cases, scratching the affected area may lead to breaks in the skin, creating an entry point for bacteria. This can result in a secondary bacterial infection alongside the fungal infection.
In conclusion, jock itch is a common fungal infection that can cause discomfort and irritation in the groin area. Maintaining good personal hygiene, wearing breathable clothing, and promptly addressing symptoms with antifungal medications are key components of effective management. For persistent or severe cases, seeking guidance from healthcare professionals ensures accurate diagnosis and appropriate treatment for a quicker resolution of symptoms.
Psoriasis

Psoriasis
Psoriasis: Unraveling Symptoms, Causes, and Types
Psoriasis is a chronic autoimmune skin condition characterized by the rapid buildup of skin cells, leading to the formation of thick, red, and scaly patches. This condition affects both the skin and, in some cases, the joints. Understanding the symptoms, causes, and types of psoriasis is crucial for effective management and improved quality of life.
Symptoms:
- Red Patches of Skin:
– Psoriasis typically presents as red, raised patches of skin covered with silvery-white scales. These patches, known as plaques, can appear anywhere on the body.
- Itching and Discomfort:
– The affected skin may be itchy and uncomfortable, causing irritation and distress.
- Nail Changes:
– Psoriasis can affect the nails, causing changes such as pitting (small dents or depressions), discoloration, and separation from the nail bed.
- Joint Pain and Swelling:
– In some cases, individuals with psoriasis may experience joint pain and swelling, a condition known as psoriatic arthritis.
- Dry or Cracked Skin:
– The skin affected by psoriasis may become dry, cracked, and prone to bleeding.
- Burning Sensation:
– Some individuals report a burning sensation on the skin affected by psoriasis.
Causes:
- Autoimmune Response:
– Psoriasis is considered an autoimmune disease, where the immune system mistakenly attacks healthy skin cells, causing an accelerated growth and accumulation of skin cells.
- Genetic Factors:
– There is a genetic predisposition to psoriasis, and individuals with a family history of the condition are at a higher risk.
- Environmental Triggers:
– Certain environmental factors, such as stress, infections, or injuries to the skin, can trigger or exacerbate psoriasis in genetically susceptible individuals.
- Immune System Dysregulation:
– Abnormal functioning of the immune system, particularly involving T cells, plays a significant role in the development of psoriasis.
- Inflammatory Response:
– Psoriasis is associated with an overactive inflammatory response, leading to the characteristic symptoms of redness, swelling, and scaling.
Types:
- Plaque Psoriasis (Psoriasis Vulgaris):
– The most common form, characterized by raised, red patches covered with a silvery-white buildup of dead skin cells. These plaques can occur on any part of the body.
- Guttate Psoriasis:
– Common in children and young adults, guttate psoriasis manifests as small, red spots resembling drops. It is often triggered by bacterial infections, such as strep throat.
- Inverse Psoriasis:
– Affecting areas with skin folds, such as the armpits, groin, and under the breasts, inverse psoriasis appears as smooth, red lesions without the typical scaling.
- Pustular Psoriasis:
– Characterized by the presence of pus-filled blisters (pustules) on red skin. Pustular psoriasis can be localized or generalized and may be associated with systemic symptoms like fever.
- Erythrodermic Psoriasis:
– A rare but severe form, erythrodermic psoriasis involves widespread redness and scaling of the skin. It can cause significant discomfort and may be accompanied by systemic symptoms, requiring immediate medical attention.
- Nail Psoriasis:
– Psoriasis can affect the nails, causing changes such as pitting, discoloration, and separation from the nail bed. Nail psoriasis can be challenging to treat.
- Psoriatic Arthritis:
– Psoriatic arthritis is a type of inflammatory arthritis associated with psoriasis. It affects the joints and may cause pain, swelling, and stiffness. It can affect any joint, including the spine.
In conclusion, psoriasis is a multifaceted condition affecting the skin and, in some cases, the joints. While it can pose challenges, effective management strategies exist, providing relief and improving the quality of life for individuals with psoriasis. Seeking professional medical advice for accurate diagnosis and tailored treatment plans is essential for those experiencing symptoms of psoriasis.
Ringworm

Ringworm
Ringworm: Unraveling Symptoms, Causes, and Types
Ringworm, despite its name, is not caused by a worm but rather by various types of fungi. This common and contagious skin infection can affect different parts of the body, leading to distinct symptoms. Understanding the symptoms, causes, and types of ringworm is crucial for effective treatment and prevention.
Symptoms:
- Red, Circular Rash:
– The most distinctive symptom of ringworm is a red, circular rash on the skin. The rash often has raised edges and a clearer center, resembling a ring, which is how the condition got its name.
- Itching:
– Intense itching is a common symptom of ringworm. The affected area may be uncomfortable and irritated, leading to scratching and potential further spread of the infection.
- Scaling or Cracking of the Skin:
– The skin within the ring may exhibit scaling or cracking, and it can become dry and flaky.
- Blistering:
– In some cases, ringworm may cause small, fluid-filled blisters within the affected area.
- Hair Loss (if on the Scalp):
– When ringworm affects the scalp, it can lead to hair loss within the circular patches. This condition is known as tinea capitis.
- Nail Changes (if on the Nails):
– Ringworm can also affect the nails, causing changes such as thickening, discoloration, and brittleness. This form is called tinea unguium or onychomycosis.
Causes:
- Fungal Infection:
– Ringworm is caused by various fungi known as dermatophytes. These fungi thrive on the keratin found in the skin, hair, and nails.
- Direct Contact:
– The most common mode of transmission is direct skin-to-skin contact with an infected person or pet. Sharing personal items like towels, combs, or clothing can also facilitate transmission.
- Contaminated Surfaces:
– Fungi responsible for ringworm can survive on surfaces such as floors, shower stalls, and mats. Coming into contact with these contaminated surfaces can lead to infection.
- Animals:
– Pets, particularly cats and dogs, can carry the fungi that cause ringworm. Direct contact with an infected animal or exposure to their fur can result in transmission.
- Warm and Humid Environments:
– Fungi thrive in warm and humid environments. Places like locker rooms, swimming pools, and communal showers can provide an ideal breeding ground for these organisms.
Types:
- Tinea Corporis (Body Ringworm):
– This type affects the skin on the body, excluding the scalp, beard, feet, and groin. It typically presents as red, circular patches with raised edges and a clear center.
- Tinea Capitis (Scalp Ringworm):
– Tinea capitis affects the scalp and hair. It can lead to hair loss, scaling, and the development of black dots where the hair has broken off.
- Tinea Cruris (Jock Itch):
– Primarily affecting the groin area, tinea cruris manifests as red or brownish patches with raised edges. It is more common in males and is often associated with sweating and friction.
- Tinea Pedis (Athlete’s Foot):
– Athlete’s foot affects the feet, particularly the spaces between the toes. It can cause itching, burning, and peeling of the skin.
- Tinea Unguium (Onychomycosis):
– Onychomycosis affects the nails, leading to changes such as thickening, discoloration, and brittleness. It can affect both fingernails and toenails.
- Tinea Barbae (Barber’s Itch):
– Common in men with beards, tinea barbae affects facial hair follicles, leading to red, itchy patches on the beard and surrounding areas.
- Tinea Manuum (Hand Ringworm):
– Hand ringworm affects the palms and the spaces between the fingers. It can cause redness, scaling, and itching.
- Tinea Faciei (Face Ringworm):
– This type affects the face, excluding the beard area. It can present with red, circular patches and may be mistaken for other facial rashes.
Scabies

Scabies
Scabies: Unraveling Symptoms, Causes, and Types
Scabies is a highly contagious skin infestation caused by the Sarcoptes scabiei mite. This microscopic parasite burrows into the upper layer of the skin, leading to the development of an itchy rash and other characteristic symptoms. Understanding the symptoms, causes, and types of scabies is essential for prompt diagnosis and effective treatment.
Symptoms:
- Intense Itching:
– The hallmark symptom of scabies is intense itching, which is often worse at night. This itching is a result of the mites burrowing into the skin and the body’s immune response.
- Rash:
– A rash is a common feature of scabies, characterized by small, red bumps or pimple-like lesions. The rash may be accompanied by red, inflamed tracks or burrows, where the mites have tunneled under the skin.
- Sores and Crusts:
– Scratching the itchy areas can lead to the development of sores and crusts on the skin. Secondary bacterial infections may occur due to the broken skin.
- Pimple-Like Bumps:
– Scabies can cause the appearance of tiny, raised, and reddish or flesh-colored bumps on the skin, especially in the areas where the mites have burrowed.
- Linear Burrows:
– Burrows created by the mites are often seen as thin, wavy, and dark lines on the skin, commonly found in the folds of the skin, between fingers, on the wrists, elbows, or genitals.
- Inflammation and Redness:
– Inflammatory changes in the skin, including redness and swelling, are typical symptoms of scabies due to the mites’ presence and the body’s immune reaction.
Causes:
- Sarcoptes Scabiei Mite:
– Scabies is caused by infestation with the Sarcoptes scabiei mite. Female mites burrow into the outer layer of the skin to lay their eggs, triggering an immune response and causing the characteristic symptoms.
- Direct Skin-to-Skin Contact:
– Scabies is primarily transmitted through direct, prolonged skin-to-skin contact with an infected person. This can occur during close personal contact, such as holding hands or sexual contact.
- Infested Bedding or Clothing:
– While less common, scabies mites can survive for a short period away from the human body. Infestation can occur through contact with infested bedding, towels, or clothing.
- Crowded Living Conditions:
– Scabies is more prevalent in environments where people live closely together, such as nursing homes, prisons, or crowded households. The mites can easily spread in such conditions.
- Mother-to-Child Transmission:
– Infants and young children may contract scabies through close contact with an infected parent or caregiver. The mites can also be transmitted during breastfeeding.
- Sexual Transmission:
– Sexual contact is a common mode of transmission for scabies in adults. Genital scabies may involve burrows and rashes in the genital and pubic areas.
Types:
- Classic Scabies:
– Classic scabies is the most common form, characterized by the presence of burrows, rashes, and intense itching. It can affect various parts of the body, including the hands, wrists, elbows, genital area, and buttocks.
- Crusted (Norwegian) Scabies:
– Crusted scabies is a more severe and less common form, especially seen in individuals with weakened immune systems. The mite infestation is more extensive, and thick, crusted lesions with a high number of mites may develop.
- Scabies in Infants and Children:
– Scabies in infants and children may present with a widespread rash, including on the face, neck, palms, and soles. It can be challenging to diagnose in this age group, and close contacts may also need treatment.
- Genital Scabies:
– Genital scabies specifically affects the genital and pubic areas. It is often transmitted through sexual contact and may present with burrows, rashes, and itching in the genital region.
- Nodular Scabies:
– Nodular scabies is characterized by the development of firm, raised nodules under the skin. These nodules are a result of the body’s reaction to the presence of scabies mites.
Seborrhoeic Dermatitis

Seborrhoeic Dermatitis
Seborrheic Dermatitis: Unraveling Symptoms, Causes, and Types
Seborrheic dermatitis is a common skin condition characterized by red, itchy, and flaky patches, typically on areas of the body where sebaceous (oil) glands are more prominent. While not a serious medical condition, it can be chronic and recurrent, causing discomfort and affecting the quality of life. Understanding the symptoms, causes, and types of seborrheic dermatitis is crucial for effective management and relief.
Symptoms:
- Red, Inflamed Skin:
– Seborrheic dermatitis often presents with red or pink patches of skin, particularly in areas rich in sebaceous glands, such as the face, scalp, and upper chest.
- Scaly, Flaky Skin:
– A hallmark of this condition is the presence of yellowish or white, greasy scales or flakes on the affected skin. The scales may vary in size and are commonly found on the scalp, eyebrows, and behind the ears.
- Itching and Irritation:
– Itching is a common symptom, and scratching the affected areas can exacerbate inflammation and lead to secondary infections.
- Oily or Greasy Appearance:
– Skin affected by seborrheic dermatitis may appear oily or greasy due to an overproduction of sebum, the skin’s natural oil.
- Dandruff:
– On the scalp, seborrheic dermatitis often manifests as dandruff, with visible flakes of skin in the hair or on clothing.
- Rash in Skin Folds:
– In some cases, seborrheic dermatitis can occur in skin folds, such as those around the nose, under the breasts, or in the groin area, resulting in a rash.
Causes:
- Yeast Overgrowth (Malassezia):
– The yeast Malassezia is naturally present on the skin but can proliferate in individuals with seborrheic dermatitis. The yeast’s interaction with sebum triggers an inflammatory response.
- Genetic Predisposition:
– A genetic predisposition may contribute to an increased susceptibility to seborrheic dermatitis. Individuals with a family history of the condition may be more prone to developing it.
- Hormonal Factors:
– Changes in hormone levels, such as those occurring during puberty, pregnancy, or with certain medical conditions, may influence the development of seborrheic dermatitis.
- Neurological Factors:
– Neurological conditions, including Parkinson’s disease, have been associated with an increased risk of seborrheic dermatitis.
- Immune System Response:
– The immune system’s response to the presence of Malassezia or other factors on the skin may contribute to the inflammatory nature of seborrheic dermatitis.
- Environmental Factors:
– Harsh weather conditions, especially cold and dry weather, can exacerbate seborrheic dermatitis symptoms. Stress and fatigue can also play a role.
Types:
- Scalp Seborrheic Dermatitis (Dandruff):
– One of the most common types, it causes flaky skin on the scalp, often resulting in dandruff. The condition may extend to the forehead, ears, and neck.
- Facial Seborrheic Dermatitis:
– This type affects the face, particularly the areas around the nose, eyebrows, and behind the ears. Redness, scaling, and greasy skin are typical features.
- Seborrheic Dermatitis on the Chest and Back:
– Seborrheic dermatitis can extend to the upper chest and back, presenting as red, scaly patches. This form may be mistaken for other skin conditions, such as psoriasis.
- Infantile Seborrheic Dermatitis (Cradle Cap):
– Common in infants, cradle cap manifests as thick, yellow or brown scales on the scalp. It is generally harmless and tends to resolve on its own.
- Seborrheic Dermatitis in Skin Folds:
– Skin folds, such as those around the nose, under the breasts, and in the groin area, can be affected, leading to a rash with redness and scaling.
Skin allergy

Skin allergy
Skin Allergy: Unraveling Symptoms, Causes, and Types
Skin allergies, also known as allergic dermatitis, are hypersensitive reactions of the skin to certain substances, typically harmless, referred to as allergens. These allergies can manifest in various forms and range from mild itching to severe rashes and inflammation. Understanding the symptoms, causes, and types of skin allergies is essential for accurate diagnosis and effective management.
Symptoms:
- Itching (Pruritus):
– Itching is a common and often the first symptom of skin allergies. It can range from mild to severe and may lead to scratching, exacerbating the condition.
- Redness (Erythema):
– Allergic reactions can cause redness of the skin, giving it a flushed appearance. The intensity of redness varies depending on the severity of the allergy.
- Rash or Hives:
– Skin allergies often manifest as rashes or hives, which are raised, swollen welts on the skin. These can be itchy and may vary in size and shape.
- Dry or Scaly Skin:
– Dryness and scaliness of the skin are common symptoms, especially when the allergen disrupts the skin’s natural barrier function.
- Inflammation:
– Allergic dermatitis can lead to inflammation, causing swelling and tenderness in the affected areas.
- Blistering:
– In some cases, skin allergies may result in the formation of blisters filled with fluid, adding to the discomfort.
- Oozing or Crusting:
– Allergic reactions may lead to oozing of clear or yellow fluid from affected areas. As the condition progresses, crusting may occur.
- Pain or Discomfort:
– Pain or discomfort can be associated with more severe skin allergies, particularly when the skin is inflamed or blistered.
Causes:
- Contact Dermatitis:
– Contact dermatitis is one of the most common types of skin allergy. It occurs when the skin comes into direct contact with an allergen or irritant. Common triggers include certain cosmetics, fragrances, metals (nickel), and cleaning products.
- Atopic Dermatitis (Eczema):
– Atopic dermatitis, often referred to as eczema, is a chronic skin condition characterized by dry, itchy skin. Genetic and environmental factors contribute to its development, and triggers may include allergens, stress, and climate changes.
- Allergic Reaction to Medications:
– Certain medications can trigger allergic reactions leading to skin symptoms. Antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), and anticonvulsants are examples of medications that may cause skin allergies.
- Insect Bites and Stings:
– Allergic reactions to insect bites or stings, such as those from bees, wasps, or mosquitoes, can result in localized or widespread skin allergies.
- Food Allergies:
– Some individuals may experience skin allergies as a result of food allergies. Common allergens include nuts, shellfish, dairy, and certain fruits.
- Latex Allergy:
– Latex allergy can cause skin reactions in individuals sensitive to latex products, such as gloves or medical devices.
- Plant Allergies:
– Contact with certain plants, including poison ivy, poison oak, or poison sumac, can lead to allergic contact dermatitis characterized by a red, itchy rash.
Types:
- Contact Dermatitis:
– Contact dermatitis is divided into irritant contact dermatitis and allergic contact dermatitis. Irritant contact dermatitis occurs when the skin is exposed to a substance causing irritation, while allergic contact dermatitis involves an immune response to an allergen.
- Atopic Dermatitis (Eczema):
– Atopic dermatitis is a chronic skin condition associated with a compromised skin barrier, leading to dry, itchy skin. It often develops in childhood but can persist into adulthood.
- Urticaria (Hives):
– Urticaria, commonly known as hives, is characterized by raised, red, itchy welts on the skin. It can be triggered by various allergens, including foods, medications, or insect stings.
- Angioedema:
– Angioedema involves swelling in deeper layers of the skin, often around the eyes and lips. It can occur alongside urticaria and is sometimes associated with more severe allergic reactions.
- Nummular Dermatitis:
– Nummular dermatitis is a form of dermatitis characterized by coin-shaped lesions on the skin. While the exact cause is not always clear, it can be associated with skin dryness and irritants.
- Stasis Dermatitis:
– Stasis dermatitis is typically associated with poor circulation and occurs in the lower legs. It is characterized by redness, scaling, and swelling.
- Seborrheic Dermatitis:
– Seborrheic dermatitis is a chronic condition that affects areas with a high concentration of sebaceous glands. It can cause red, scaly patches on the scalp, face, and other areas.
Skin Blemishes Treatment

Skin Blemishes Treatment
Skin Blemishes: Unraveling Symptoms, Causes, and Types
Skin blemishes refer to imperfections or irregularities on the skin’s surface, often characterized by discoloration, spots, or other visual alterations. These blemishes can arise from various factors, including acne, sun exposure, aging, or underlying skin conditions. Understanding the symptoms, causes, and types of skin blemishes is essential for effective management and maintaining healthy skin.
Symptoms:
- Discoloration:
– Skin blemishes often manifest as areas of discoloration, appearing darker or lighter than the surrounding skin. This can result from pigmentation irregularities or inflammation.
- Spots or Lesions:
– Blemishes may present as spots, lesions, or irregularities on the skin’s surface. These can vary in size, shape, and texture.
- Redness or Inflammation:
– Inflammatory conditions, such as acne or dermatitis, may lead to redness and inflammation, contributing to the appearance of blemishes.
- Scarring:
– Previous skin injuries or conditions can result in scarring, which may be considered a type of skin blemish. Scars can range from subtle to more pronounced.
- Uneven Texture:
– Blemishes may alter the texture of the skin, leading to unevenness or rough patches.
- Enlarged Pores:
– Conditions like acne can contribute to enlarged pores, which may be considered a type of skin blemish.
Causes:
- Acne:
– One of the most common causes of skin blemishes is acne, which occurs when hair follicles become clogged with oil and dead skin cells. Acne lesions can include whiteheads, blackheads, pimples, or cysts.
- Sun Exposure:
– Prolonged exposure to ultraviolet (UV) radiation from the sun can lead to sun damage, causing dark spots, freckles, or uneven pigmentation.
- Aging:
– Aging can contribute to the development of blemishes, including wrinkles, fine lines, and age spots. Reduced collagen production and slower skin cell turnover are factors in this process.
- Skin Infections:
– Bacterial, viral, or fungal infections can cause skin blemishes. Conditions like impetigo or fungal infections can lead to visible spots or lesions.
- Inflammatory Skin Conditions:
– Conditions such as eczema, psoriasis, or contact dermatitis can cause redness, inflammation, and other blemishes on the skin.
- Hormonal Changes:
– Fluctuations in hormones, such as those that occur during puberty, pregnancy, or menopause, can contribute to skin blemishes. Hormonal acne is a common manifestation.
- Genetic Factors:
– Genetic predispositions may influence an individual’s susceptibility to certain skin conditions, including those leading to blemishes.
- Poor Skincare Habits:
– Inadequate skincare practices, including improper cleansing, using harsh products, or neglecting sunscreen, can contribute to skin blemishes.
Types:
- Acne Blemishes:
– Acne blemishes encompass various types, including whiteheads (closed comedones), blackheads (open comedones), papules, pustules, nodules, and cysts. Each represents a different stage or type of acne lesion.
- Age Spots (Liver Spots):
– Age spots, also known as liver spots, are flat, brown, or grayish spots that develop on sun-exposed areas of the skin due to prolonged UV exposure. They are common in older adults.
- Sun Spots (Solar Lentigines):
– Sun spots, or solar lentigines, are pigmented spots that result from sun damage. They are darker than the surrounding skin and often appear on areas exposed to the sun.
- Freckles:
– Freckles are small, concentrated areas of increased pigmentation. They are often genetic and become more noticeable with sun exposure.
- Melasma:
– Melasma is a condition characterized by brown or gray-brown patches on the face, often associated with hormonal changes during pregnancy or birth control use.
- Post-Inflammatory Hyperpigmentation (PIH):
– PIH occurs after skin inflammation or injury, such as acne, and results in dark spots or discoloration. It’s more common in individuals with darker skin tones.
- Scars:
– Scars, which can be caused by injuries, surgeries, or certain skin conditions, represent a lasting alteration in the skin’s structure and can be considered a type of blemish.
- Eczema Blemishes:
– Eczema can cause red, inflamed, and itchy patches on the skin. Over time, these patches may thicken, resulting in blemishes.
Skin disease

Skin disease
Skin Diseases: Overview of Symptoms, Causes, and Types
Skin diseases encompass a broad range of conditions affecting the skin, with diverse symptoms, causes, and types. These disorders can be caused by various factors, including genetics, infections, autoimmune responses, environmental elements, or underlying health conditions.
Symptoms:
- Rashes and Redness:
– Many skin diseases present with noticeable rashes, alterations in skin color, and areas of redness, indicating underlying inflammation.
- Itching (Pruritus):
– Persistent itching is a common symptom, often leading to discomfort and skin irritation. Itching can vary in intensity depending on the specific skin condition.
- Pain or Discomfort:
– Skin diseases may cause pain or discomfort, especially in conditions involving inflammation, infections, or lesions.
- Scaling or Peeling:
– Scaling or peeling of the skin is common in certain skin diseases, such as psoriasis or fungal infections, resulting in flaky or shedding skin.
- Blisters or Lesions:
– The presence of blisters or lesions is indicative of various skin diseases, including autoimmune disorders or viral infections.
Causes:
- Genetics:
– Genetic factors contribute significantly to several skin diseases, such as psoriasis, eczema, or hereditary forms of skin cancer.
- Infections:
– Bacterial, viral, or fungal infections can cause a range of skin diseases, including impetigo, warts, or ringworm.
- Autoimmune Responses:
– Autoimmune disorders, where the immune system mistakenly attacks healthy cells, can lead to skin diseases like lupus or scleroderma.
- Environmental Factors:
– Exposure to environmental elements, such as allergens, pollutants, or harsh weather conditions, can contribute to skin diseases like contact dermatitis or environmental allergies.
Types:
- Acne:
– Acne is a common skin disease characterized by the development of pimples, blackheads, and cysts. It often occurs during puberty due to hormonal changes.
- Eczema (Dermatitis):
– Eczema encompasses various inflammatory skin conditions, causing redness, itching, and sometimes blistering. Atopic dermatitis is a common form.
- Psoriasis:
– Psoriasis is a chronic autoimmune condition resulting in raised, red, and scaly patches due to rapid skin cell turnover.
- Rosacea:
– Rosacea is a chronic skin disease marked by redness, visible blood vessels, and sometimes pimple-like bumps, commonly affecting the face.
- Skin Cancer:
– Skin cancer, including basal cell carcinoma, squamous cell carcinoma, and melanoma, results from the uncontrolled growth of skin cells.
- Viral Infections:
– Viral infections, such as herpes simplex or human papillomavirus, can cause skin diseases like cold sores, warts, or genital warts.
- Fungal Infections:
– Fungal infections, like ringworm or athlete’s foot, are common skin diseases caused by various fungi.
In conclusion, skin diseases are diverse and can manifest with varying symptoms and causes. Timely diagnosis and appropriate management are essential for maintaining skin health and preventing complications. If individuals notice persistent or concerning skin changes, seeking medical advice is crucial for an accurate diagnosis and tailored treatment.
Sun Burn

Sun Burn
Sunburn: Unveiling Symptoms, Causes, and Types
Sunburn is a skin condition caused by overexposure to ultraviolet (UV) radiation from the sun or other artificial sources like tanning beds. While it is often a temporary and minor issue, severe sunburn can lead to complications. Understanding the symptoms, causes, and types of sunburn is crucial for effective prevention and management.
Symptoms:
- Redness:
– The most noticeable symptom of sunburn is redness of the affected skin. This occurs due to increased blood flow to the area in response to UV damage.
- Pain and Tenderness:
– Sunburned skin is often painful and tender to the touch. This discomfort is a result of inflammation caused by UV radiation.
- Swelling:
– Swelling can accompany severe sunburn, contributing to the overall discomfort. It is a sign of inflammation and the body’s response to tissue damage.
- Blistering:
– In more severe cases, sunburn can lead to the formation of blisters filled with fluid. These blisters can increase the risk of infection if not properly cared for.
- Peeling:
– As the skin begins to heal, sunburned areas may start to peel. This is a natural part of the body’s process of shedding damaged skin cells.
- Itching:
– Sunburned skin can be itchy, especially during the peeling phase. Scratching can further irritate the skin and delay the healing process.
- Fatigue and Malaise:
– Systemic symptoms like fatigue and malaise may occur, especially in cases of extensive sunburn. Dehydration and the body’s response to inflammation contribute to these symptoms.
Causes:
- Ultraviolet (UV) Radiation:
– Sunburn is primarily caused by exposure to UV radiation from the sun. UV radiation damages the DNA in skin cells, triggering a defensive inflammatory response.
- Sun Intensity:
– Sunburn risk increases in areas with high sun intensity, especially during peak hours (10 a.m. to 4 p.m.). Altitude and proximity to the equator also affect UV exposure.
- Skin Type:
– Individuals with fair or light skin are more susceptible to sunburn. People with darker skin have more melanin, providing some natural protection against UV damage.
- Lack of Sunscreen:
– Insufficient or improper use of sunscreen increases the risk of sunburn. Sunscreen with a high SPF should be applied generously and reapplied regularly, especially after swimming or sweating.
- Medications:
– Certain medications, such as some antibiotics, diuretics, and acne medications, can increase sensitivity to UV radiation, making individuals more prone to sunburn.
- Reflective Surfaces:
– Water, sand, snow, and other reflective surfaces can intensify UV exposure. Sunburn risk is higher in environments where UV rays are reflected onto the skin.
Types:
- First-Degree Sunburn (Superficial):
– This is the mildest form of sunburn, characterized by redness, pain, and tenderness. Peeling may occur during the healing process, but blisters are typically absent.
- Second-Degree Sunburn (Partial Thickness):
– Second-degree sunburn is more severe, involving deeper layers of the skin. Blisters may develop, and the pain and swelling are more pronounced. Healing may take longer than with first-degree sunburn.
- Severe Sunburn (Sun Poisoning):
– Sun poisoning is an extreme form of sunburn associated with severe symptoms, including extensive blistering, fever, chills, nausea, and dehydration. It requires prompt medical attention.
- Chronic Sun Damage:
– Prolonged, repeated sun exposure can lead to chronic sun damage, contributing to premature aging and an increased risk of skin cancers.
Tinea alba

Tinea alba
Tinea Alba: Decoding Symptoms, Causes, and Types
Tinea alba is a common skin condition that typically affects children and adolescents. It is a type of superficial fungal infection that manifests as dry, hypopigmented, scaly patches on the skin. Understanding the symptoms, causes, and types of tinea alba is crucial for accurate diagnosis and effective treatment.
Symptoms:
- Hypopigmented Patches:
– The primary symptom of tinea alba is the presence of light-colored, hypopigmented patches on the skin. These patches may be round or oval and are usually lighter than the surrounding skin.
- Dry and Scaly Skin:
– Tinea alba often presents with dry and scaly skin on the affected patches. The skin may appear flaky, giving it a texture that is different from the surrounding normal skin.
- Mild Itching:
– Itching is a common symptom, but it is usually mild. Individuals with tinea alba may experience occasional itching on the affected areas.
- Circular or Oval Shape:
– The patches of tinea alba are often circular or oval in shape. They may vary in size and can occur on different parts of the body.
- Face, Neck, and Upper Arms:
– Tinea alba commonly occurs on the face, particularly the cheeks, neck, and upper arms. However, it can also affect other areas of the body.
Causes:
- Fungal Infection (Tinea):
– Tinea alba is caused by a superficial fungal infection. The specific fungus involved is often a type of dermatophyte, such as Trichophyton or Microsporum.
- Predisposing Factors:
– Certain factors predispose individuals to tinea alba, including a warm and humid climate, excessive sweating, and sharing personal items like towels or clothing.
- Atopy (Genetic Predisposition):
– Individuals with a genetic predisposition to atopic conditions, such as eczema or asthma, may be more prone to developing tinea alba.
- Weakened Immune System:
– A compromised immune system can increase the risk of fungal infections, including tinea alba. This may be seen in individuals with conditions like HIV or those undergoing immunosuppressive therapy.
- Poor Hygiene Practices:
– Poor hygiene practices, especially in warm and humid conditions, can contribute to the development and spread of fungal infections.
- Excessive Sun Exposure:
– Sun exposure can exacerbate the hypopigmentation associated with tinea alba, making the affected patches more noticeable.
Types:
- Tinea Versicolor:
– Tinea versicolor is a type of fungal infection caused by the yeast Malassezia. It typically presents as discolored patches on the skin, which can be either lighter or darker than the surrounding skin. While tinea versicolor is distinct from tinea alba, they share some similarities.
- Tinea Corporis (Ringworm):
– Tinea corporis, commonly known as ringworm, is a fungal infection that can affect various parts of the body, including the face, neck, and arms. It may present as red, circular, and scaly patches, sometimes with an elevated border.
- Atopic Dermatitis (Eczema):
– Atopic dermatitis, or eczema, is a chronic skin condition characterized by inflammation and itching. While eczema is not a fungal infection, its appearance can be similar to tinea alba, especially during flares.
Tinea Rosea

Tinea Rosea
Tinea Rosea: Unveiling Symptoms, Causes, and Types
Tinea rosea is a common skin condition characterized by the appearance of distinctive rash-like lesions. While its exact cause remains unclear, it is believed to be associated with viral infections. Understanding the symptoms, causes, and types of tinea rosea is essential for accurate diagnosis and appropriate management.
Symptoms:
- Herald Patch:
– Tinea rosea often begins with a single, larger lesion called the “herald patch.” This patch is typically round or oval and may have a scaly or raised border. It is usually the first sign of the condition.
- Secondary Patches:
– Following the appearance of the herald patch, smaller patches develop on different parts of the body. These secondary patches are smaller in size and may form a distinctive pattern that resembles the branches of a tree or an inverted Christmas tree.
- Itching:
– Many individuals with tinea rosea experience itching, particularly in the early stages of the condition. The itching may vary in intensity and can be bothersome for some individuals.
- General Malaise:
– Some people may experience general malaise, which includes feelings of fatigue, weakness, or discomfort. However, systemic symptoms are generally mild.
- Fever and Headache (Rare):
– In rare cases, individuals with tinea rosea may experience mild systemic symptoms such as fever and headache. However, these symptoms are not common.
Causes:
- Viral Infections:
– Tinea rosea is thought to be associated with viral infections, with human herpesvirus (HHV-6 and HHV-7) often suspected as potential triggers. However, the exact relationship between tinea rosea and viral infections is not fully understood.
- Immune Response:
– The development of tinea rosea may involve an immune response to a viral infection, leading to the characteristic skin lesions. However, the immune mechanisms underlying tinea rosea are still a subject of research.
- Environmental Factors:
– Environmental factors, such as changes in weather or humidity, may contribute to the development of tinea rosea, although their role is not well-defined.
- Hormonal Factors:
– Some cases of tinea rosea have been reported to occur more frequently in certain age groups, suggesting potential hormonal influences. However, more research is needed to establish clear associations.
- Genetic Predisposition:
– While there is no direct evidence of a genetic predisposition to tinea rosea, some individuals may be more susceptible to certain viral infections, contributing to their likelihood of developing this skin condition.
Types:
- Classic Tinea Rosea:
– Classic tinea rosea follows the typical course, starting with the appearance of the herald patch followed by smaller secondary patches. The rash is usually self-limiting and resolves within a few weeks to months.
- Inverse Tinea Rosea:
– Inverse tinea rosea is a variant where the rash appears in skin folds or areas with increased moisture, such as the armpits, groin, or under the breasts. This variant may present with more pronounced itching due to the location of the lesions.
- Gibert-Type Tinea Rosea:
– Gibert-type tinea rosea is a less common variant that may have atypical features. The lesions in this variant may differ in appearance or distribution compared to classic tinea rosea.
- Relapsing Tinea Rosea:
– In relapsing tinea rosea, individuals experience recurrent episodes of the characteristic rash over time. The reasons for the recurrence are not well understood.
Tinea Versicolor

Tinea Versicolor
Tinea Versicolor: Unveiling Symptoms, Causes, and Types
Tinea versicolor is a common skin condition caused by an overgrowth of the yeast Malassezia on the skin. While the condition is usually harmless, it can cause noticeable changes in skin color and texture. Understanding the symptoms, causes, and types of tinea versicolor is crucial for accurate diagnosis and effective treatment.
Symptoms:
- Hypopigmented or Hyperpigmented Patches:
– Tinea versicolor typically presents as patches on the skin that are lighter (hypopigmented) or darker (hyperpigmented) than the surrounding skin. The patches may vary in size and shape.
- Scaling and Flaking:
– Affected areas often exhibit fine scaling and flaking, creating a surface that may resemble a fine layer of powder on the skin.
- Mild Itching:
– Itching is usually mild, but some individuals may experience discomfort or irritation in the affected areas.
- Worsening in Heat or Humidity:
– Symptoms of tinea versicolor often worsen in warm and humid conditions. Increased sweating can contribute to the overgrowth of Malassezia.
- Common Areas of Involvement:
– Tinea versicolor commonly affects areas with a high concentration of sebaceous (oil) glands, such as the chest, back, neck, upper arms, and shoulders.
Causes:
- Malassezia Yeast Overgrowth:
– The primary cause of tinea versicolor is the overgrowth of the yeast Malassezia on the skin. This yeast is a normal component of the skin’s microbiota, but an overgrowth can lead to the characteristic skin changes.
- Warm and Humid Environments:
– Tinea versicolor is more common in regions with warm and humid climates. Increased heat and humidity create favorable conditions for the overgrowth of Malassezia.
- Oily Skin:
– Excessively oily or seborrheic skin is associated with an increased risk of tinea versicolor. The yeast Malassezia thrives on the lipids present in sebum, contributing to its overgrowth.
- Immunosuppression:
– Conditions or medications that suppress the immune system can increase the risk of tinea versicolor. This includes conditions like HIV/AIDS or the use of immunosuppressive medications.
- Hormonal Changes:
– Hormonal changes, such as those occurring during puberty, pregnancy, or while taking oral contraceptives, can influence the likelihood of developing tinea versicolor.
Types:
- Hypopigmented Tinea Versicolor:
– Hypopigmented tinea versicolor is characterized by patches that are lighter than the surrounding skin. These patches can be more noticeable in individuals with darker skin tones.
- Hyperpigmented Tinea Versicolor:
– Hyperpigmented tinea versicolor involves patches that are darker than the surrounding skin. This type may be more noticeable in individuals with lighter skin tones.
- Mixed Presentation:
– Some cases of tinea versicolor may present with a combination of hypopigmented and hyperpigmented patches on the skin.
Urticaria

Urticaria
Urticaria: Understanding Symptoms, Causes, and Types
Urticaria, commonly known as hives, is a skin condition characterized by the sudden appearance of itchy, raised welts on the skin. These welts, also known as wheals or hives, can vary in size and shape and often cause discomfort. Understanding the symptoms, causes, and types of urticaria is essential for effective management and relief.
Symptoms:
- Raised Welts (Hives):
– The hallmark symptom of urticaria is the sudden appearance of raised, red or skin-colored welts on the surface of the skin. These welts can be small or large and may merge to form larger areas of swelling.
- Itching (Pruritus):
– Urticaria is typically accompanied by intense itching, which can be bothersome and contribute to the overall discomfort experienced by individuals with hives.
- Redness and Swelling:
– The affected skin becomes red and swollen due to the inflammatory response triggered by the release of histamine.
- Blanching:
– When pressure is applied to the center of a hive, it often blanches or turns white. This characteristic helps differentiate urticaria from other skin conditions.
- Transient Nature:
– Urticaria is known for its transient nature. Individual hives usually last for a short duration before resolving, but new ones may continue to appear.
Causes:
- Allergic Reactions:
– Allergic reactions to certain foods, medications, insect stings, or latex can trigger urticaria. The body releases histamine in response to the allergen, leading to the characteristic welts and itching.
- Infections:
– Infections, especially viral or bacterial infections, can stimulate the immune system and contribute to the development of hives.
- Autoimmune Disorders:
– Autoimmune disorders, where the immune system mistakenly targets the body’s tissues, can lead to chronic urticaria in some individuals.
- Physical Stimuli (Physical Urticaria):
– Exposure to physical stimuli such as heat, cold, pressure, or sunlight can induce urticaria in susceptible individuals. This form is known as physical urticaria.
- Stress:
– Emotional stress can trigger or exacerbate urticaria. The release of stress hormones may contribute to the release of histamine.
- Medications:
– Some medications, including antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), and certain blood pressure medications, can cause urticaria as a side effect.
- Genetic Factors:
– There may be a genetic predisposition to urticaria, as individuals with a family history of the condition may be more prone to developing hives.
Types:
- Acute Urticaria:
– Acute urticaria is characterized by the sudden onset of hives that resolve within a short period, typically lasting less than six weeks. It is often linked to allergic reactions, infections, or medication use.
- Chronic Urticaria:
– Chronic urticaria persists for more than six weeks and may last for months or even years. It can be associated with autoimmune factors, underlying medical conditions, or may have an unknown cause.
- Physical Urticaria:
– Physical urticaria is triggered by specific physical stimuli. Common types include:
– Dermatographism: Hives develop in response to scratching or pressure on the skin.
– Cold Urticaria: Exposure to cold temperatures induces hives.
– Cholinergic Urticaria: Triggered by an increase in body temperature, such as during exercise, stress, or hot showers.
– Solar Urticaria: Hives occur after exposure to sunlight.
- Contact Urticaria:
– Contact urticaria occurs when hives develop after direct skin contact with a specific substance, such as certain foods or chemicals.
- Aquagenic Urticaria:
– Aquagenic urticaria is a rare type where hives develop after contact with water, regardless of its temperature. This form of urticaria is exceptionally rare.
- Vibratory Urticaria:
– Vibratory urticaria is triggered by vibration or mechanical stimulation of the skin. Activities such as using a vibrating tool or riding a motorcycle can induce hives.
Urticaria Pigmentosa

Urticaria Pigmentosa
Urticaria Pigmentosa: Unraveling Symptoms, Causes, and Types
Urticaria Pigmentosa (UP) is a rare form of cutaneous mastocytosis, a group of disorders characterized by an abnormal accumulation of mast cells in the skin. UP primarily affects the skin and is most commonly seen in children, although it can also occur in adults. Understanding the symptoms, causes, and types of urticaria pigmentosa is crucial for accurate diagnosis and management.
Symptoms:
- Brownish Skin Lesions (Macules):
– The hallmark of urticaria pigmentosa is the presence of brownish skin lesions, known as macules. These macules can vary in size and may resemble freckles. They often occur on the trunk, arms, and legs.
- Itching (Pruritus):
– Intense itching is a common symptom associated with urticaria pigmentosa. The itching may be exacerbated by various triggers, such as friction or heat.
- Reddening of Lesions (Darier’s Sign):
– Gentle rubbing or scratching of the macules may lead to reddening or hive-like welts, a phenomenon known as Darier’s sign. This is a characteristic feature of urticaria pigmentosa.
- Swelling and Inflammation:
– Mast cells, which are abnormally increased in urticaria pigmentosa, can release substances that cause local swelling and inflammation around the skin lesions.
- Nausea and Vomiting:
– In some cases, individuals with urticaria pigmentosa may experience symptoms beyond the skin, such as nausea, vomiting, abdominal pain, or diarrhea. This occurs due to the release of mast cell mediators affecting other organ systems.
- Flushing:
– Flushing, or sudden redness of the face, may occur due to mast cell activation. This is more common in response to triggers like stress or alcohol.
Causes:
- Mast Cell Accumulation:
– The primary cause of urticaria pigmentosa is the abnormal accumulation and proliferation of mast cells in the skin. Mast cells are a type of immune cell involved in allergic reactions and inflammatory responses.
- Genetic Factors:
– Urticaria pigmentosa is often associated with genetic mutations in the c-KIT gene, which plays a role in the development and survival of mast cells. These mutations lead to uncontrolled mast cell growth.
- Somatic Mutations:
– The genetic mutations seen in urticaria pigmentosa are often somatic, meaning they occur in cells that are not passed on to offspring. As a result, the condition is not typically inherited.
- Triggers and Activation:
– Various triggers, such as friction, heat, stress, or exposure to certain chemicals, can cause the mast cells in the skin to release their contents, leading to the characteristic symptoms of urticaria pigmentosa.
Types:
- Solitary Mastocytoma:
– Solitary mastocytoma is a form of urticaria pigmentosa characterized by a single or a few macules or nodules. This type is often seen in infants and young children.
- Multiple Mastocytomas:
– Multiple mastocytomas involve the presence of several macules or nodules. This form is also more common in children.
- Diffuse Cutaneous Mastocytosis:
– Diffuse cutaneous mastocytosis is a severe variant where mast cell infiltration is widespread, affecting a large area of the skin. This form is typically present at birth and may be associated with systemic symptoms.
- Adult-Onset Urticaria Pigmentosa:
– While urticaria pigmentosa is more commonly diagnosed in childhood, there are instances of adult-onset cases. The symptoms and characteristics are generally similar to those seen in childhood cases.
Vitiligo

Vitiligo
Vitiligo: Unraveling Symptoms, Causes, and Types
Vitiligo is a skin disorder characterized by the loss of pigment-producing cells (melanocytes), resulting in white or depigmented patches on the skin. This condition can affect any part of the body, and while it is not harmful or contagious, it can have significant psychological and emotional impacts on individuals. Understanding the symptoms, causes, and types of vitiligo is essential for proper diagnosis and management.
Symptoms:
- Depigmented Patches:
– The primary symptom of vitiligo is the presence of depigmented or white patches on the skin. These patches may vary in size and shape and can occur on any part of the body.
- Symmetrical Distribution:
– Vitiligo often exhibits a symmetrical pattern, meaning that depigmented areas appear on both sides of the body in a mirrored fashion.
- Affected Areas:
– Common areas affected by vitiligo include the face, hands, feet, elbows, knees, genitalia, and areas around body openings (eyes, nose, mouth). It can also involve mucous membranes.
- Premature Graying of Hair:
– In addition to skin depigmentation, individuals with vitiligo may experience premature graying or whitening of hair in the affected areas.
- Symptoms Progression:
– Vitiligo is characterized by a progressive course, and new depigmented areas may appear over time. The rate at which the condition progresses varies among individuals.
- Photosensitivity:
– Some people with vitiligo may notice increased sensitivity to sunlight in the depigmented areas, leading to a higher risk of sunburn.
Causes:
- Autoimmune Factors:
– The leading theory regarding the cause of vitiligo involves an autoimmune response where the immune system mistakenly attacks and destroys melanocytes. Genetic factors may contribute to this autoimmune response.
- Genetic Predisposition:
– There is evidence suggesting a genetic predisposition to vitiligo. Individuals with a family history of vitiligo or other autoimmune conditions may be at a higher risk.
- Neurogenic Factors:
– Neurogenic factors, involving nerve damage or dysfunction, may contribute to the development of vitiligo. This theory suggests that changes in nerve function can affect the melanocytes.
- Oxidative Stress:
– Oxidative stress, caused by an imbalance between the production of reactive oxygen species and the body’s ability to neutralize them, is considered a factor in vitiligo. This oxidative stress can damage melanocytes.
- Viral or Environmental Triggers:
– While not conclusively proven, some researchers propose that viral infections or exposure to certain environmental factors may trigger vitiligo in individuals with a genetic predisposition.
Types:
- Non-Segmental Vitiligo:
Non-segmental vitiligo is the most common type, accounting for the majority of cases. It typically presents with symmetrical depigmented patches on both sides of the body. Subtypes include
– Generalized Vitiligo: Involves widespread depigmentation
– Universal Vitiligo: Almost the entire body surface is affected.
– Focal Vitiligo: Few scattered patches without a clear pattern.
- Segmental Vitiligo:
Segmental vitiligo is characterized by depigmentation that occurs on one side or a segment of the body. It often begins at a young age and progresses for a limited time. This type is less common than non-segmental vitiligo.
- Mixed Vitiligo:
Mixed vitiligo involves a combination of non-segmental and segmental patterns. Both symmetrical and asymmetrical depigmented patches may be present.
- Acrofacial Vitiligo:
Acrofacial vitiligo specifically affects the fingers and face. It commonly involves depigmentation around the eyes, nose, and mouth, as well as the fingertips.
- Mucosal Vitiligo:
Mucosal vitiligo affects the mucous membranes, leading to depigmentation in areas such as the lips, inside the mouth, and genitalia.
- Trichrome Vitiligo:
Trichrome vitiligo is characterized by the presence of three distinct colors in the depigmented areas – white, light brown, and normal skin color.
Warts

Warts
Warts: Unraveling Symptoms, Causes, and Types
Warts are noncancerous skin growths caused by the human papillomavirus (HPV). While they are generally harmless, warts can be unsightly and, in some cases, may cause discomfort. Understanding the symptoms, causes, and types of warts is essential for effective management and prevention.
Symptoms:
- Skin Growth:
– The primary symptom of warts is the presence of a raised, rough, or bumpy growth on the skin. Warts can vary in size and appearance.
- Rough Texture:
– Warts often have a rough or grainy texture, making them distinguishable from the surrounding skin.
- Color Variations:
– Warts can appear in different colors, including flesh-toned, white, pink, or brown. The color may depend on the specific type of wart and the individual’s skin tone.
- Pain or Discomfort:
– Warts are usually painless, but in some cases, they may cause discomfort, especially if they develop on pressure points like the soles of the feet (plantar warts) or on fingers.
- Clustering:
– Warts can occur singly or in clusters. Clusters of small warts are often referred to as mosaic warts.
- Black Dots:
– Some warts may have tiny black dots or pinpoint bleeding within them. These dots are often capillaries that supply blood to the wart.
Causes:
- Human Papillomavirus (HPV):
– Warts are caused by various strains of HPV, a group of viruses that infect the top layer of the skin. Different types of HPV lead to the formation of different types of warts.
- Direct Contact:
– Warts are highly contagious and can spread through direct skin-to-skin contact with an infected person or by touching surfaces that have the virus.
- Cuts or Scratches:
– Open cuts or scratches on the skin provide an entry point for the HPV virus, increasing the risk of developing warts.
- Weakened Immune System:
– Individuals with a weakened immune system, such as those with HIV/AIDS or undergoing immunosuppressive treatments, are more susceptible to developing and experiencing persistent warts.
- Wet or Damaged Skin:
– The virus thrives in moist environments, and warts are more likely to develop on wet or damaged skin.
- Nail Biting or Finger Sucking:
– Warts can occur on the fingers or around the nails, particularly in individuals who bite their nails or suck their fingers.
Types:
- Common Warts (Verruca Vulgaris):
– These are the most prevalent type of warts and often appear on the hands, fingers, and around the nails. They have a rough texture and may have black dots.
- Plantar Warts:
– Plantar warts develop on the soles of the feet and can be painful due to pressure from walking. They often have a flattened appearance and may have tiny black dots.
- Flat Warts (Verruca Plana):
– Flat warts are smoother and smaller compared to common warts. They can appear in large numbers, often on the face, neck, hands, or legs.
- Filiform Warts:
– Filiform warts have a thread-like or finger-like appearance. They often occur around the mouth, eyes, or on the neck and can be more prominent.
- Periungual Warts:
– Periungual warts develop around the nails and can affect nail growth. They may be more common in individuals who bite their nails.
- Genital Warts (Condyloma Acuminata):
– Genital warts are a sexually transmitted infection caused by certain strains of HPV. They appear on the genital and anal areas and are often flesh-colored or pink.
- Subungual and Periungual Warts:
– These warts develop under and around the toenails and fingernails. They can cause changes in nail appearance and may be painful.
- Mosaic Warts:
– Mosaic warts are clusters of small warts that often form on the hands or feet, creating a mosaic-like pattern.
Prevention involves practicing good hygiene, avoiding direct contact with warts, and not picking at or scratching existing warts to prevent their spread. It’s important to consult with a healthcare professional for appropriate diagnosis and treatment based on the type and location of the wart.
Yeast infection (Candidiasis)

Yeast infection (Candidiasis)
Yeast Infection: Unraveling Symptoms, Causes, and Types
Yeast infections, also known as candidiasis, are fungal infections caused by an overgrowth of the Candida yeast, primarily Candida albicans. While Candida is naturally present in the body, certain conditions can lead to an imbalance, resulting in an infection. Understanding the symptoms, causes, and types of yeast infections is essential for accurate diagnosis and effective management.
Symptoms:
- Genital Itching and Irritation:
– One of the most common symptoms of yeast infections in both men and women is itching and irritation in the genital area. This discomfort is often accompanied by redness and swelling.
- Vaginal Discharge:
– Women may experience an abnormal vaginal discharge that is thick, white, and resembles cottage cheese. The discharge may lack a distinct odor.
- Burning Sensation:
– A burning sensation, particularly during urination or intercourse, is a frequent symptom of yeast infections.
- Pain or Discomfort:
– Pain or discomfort in the affected area, such as the vulva in women or the penis in men, can occur.
- Redness and Swelling:
– Redness and swelling of the genital tissues are common signs, indicating inflammation due to the yeast overgrowth.
- Yeast Infections in Men:
– Men can experience yeast infections, often manifesting as redness, itching, and irritation on the penis. Discharge may also occur.
- Oral Candidiasis (Thrush):
– Yeast infections can affect the oral cavity, leading to a condition known as thrush. Symptoms include white patches on the tongue, inner cheeks, or the back of the throat, often causing discomfort and difficulty swallowing.
- Skin Candidiasis:
– In some cases, yeast infections can affect the skin, leading to red, itchy rashes with satellite lesions in areas where skin-to-skin contact occurs.
Causes:
- Immunocompromised Conditions:
– Conditions that weaken the immune system, such as HIV/AIDS or the use of immunosuppressive medications, can increase the risk of yeast infections.
- Antibiotic Use:
– The use of antibiotics can disrupt the balance of microorganisms in the body, leading to an overgrowth of Candida. Antibiotics may kill beneficial bacteria that help keep Candida in check.
- Diabetes:
– Individuals with diabetes, especially those with poorly controlled blood sugar levels, are more susceptible to yeast infections. Elevated sugar levels create an environment conducive to fungal overgrowth.
- Pregnancy:
– Hormonal changes during pregnancy, particularly increased estrogen levels, can contribute to an increased risk of yeast infections.
- Poor Personal Hygiene:
– Inadequate personal hygiene, including infrequent changing of wet or damp clothing, can create conditions favorable for yeast overgrowth.
- Diet High in Sugar:
– Diets high in sugar and refined carbohydrates provide an ample food source for Candida, promoting its growth.
- Tight Clothing:
– Wearing tight, non-breathable clothing, especially in the genital area, can create a warm and moist environment, facilitating yeast overgrowth.
- Hormonal Changes:
– Hormonal fluctuations, such as those occurring during the menstrual cycle, menopause, or while using hormonal contraceptives, can contribute to yeast infections.
- Weakened Immune Response in Elderly:
– Aging may be associated with a weakened immune response, making elderly individuals more susceptible to yeast infections.
Types:
- Vaginal Yeast Infection:
– Vaginal yeast infections are common in women and are characterized by itching, burning, and abnormal vaginal discharge. They often occur in association with factors like antibiotic use, hormonal changes, or compromised immunity.
- Oral Candidiasis (Thrush):
– Thrush affects the mouth and throat, resulting in white patches on the tongue and oral mucosa. It is commonly seen in infants, the elderly, or individuals with weakened immune systems.
- Penile Yeast Infection:
– Men can experience yeast infections on the penis, leading to redness, itching, and discomfort. Sexual transmission from an infected partner is possible.
- Cutaneous Candidiasis:
– Cutaneous candidiasis involves yeast infections of the skin, resulting in red, itchy rashes often found in skin folds or areas with skin-to-skin contact.
- Systemic Candidiasis:
– Systemic candidiasis is a more severe form of the infection where Candida enters the bloodstream. This can occur in individuals with severely compromised immune systems and may lead to widespread organ involvement.
Yeast infections are generally treatable with appropriate medical intervention. However, individuals experiencing recurrent infections or those with underlying health conditions should seek medical advice for a comprehensive evaluation and tailored management plan.
Contact to know more
Contact
Timings
Monday to Saturday:
11:00 AM to 02:30 PM
06:30 PM to 09:00 PM
